This
is part 3 of a 5 part Information Guide. Introduction:
Index
BEYOND
DIAGNOSIS - THE DESERT OF DOUBT
Having assembled
all the data available about the diagnosis, the next step is to decide what treatment
to choose - if indeed treatment is required.
It
may sound like madness not to treat a disease diagnosed as cancer immediately.
But not all cancers are equal and in many cases - probably the majority, prostate
cancer is a slow growing or indolent disease which should be managed successfully
as a chronic illness. Of course no one should ever ignore a potentially dangerous
disease, but immediate action may not be essential. All treatments for prostate
cancer have a risk of side effects (termed morbidity) which can, in many cases,
significantly reduce the quality of life. It is important to ensure as far as
possible that treatment is justified and that the most appropriate treatment is
chosen.
So...
|
WHICH TREATMENT IS THE ONE FOR ME?
When faced with this question, the
traveler
through this Strange Place will discover the greatest conundrum of the disease:
THERE IS NO AGREEMENT IN THE MEDICAL
PROFESSION AS TO WHICH TREATMENT, OR COMBINATION OF TREATMENTS, IS BEST.
Relevant
scientific data from randomized studies comparing the outcomes of various treatment
options does not exist.
|
How
can this be? This excerpt from a 1997 article in The New England Journal of
Medicine, the prestigious American medical journal, sums up the position pretty
clearly:
"... we have no firm guidelines for advising our patients about which therapeutic
option is best. This means that education is more important than ever, but the
art of multidisciplinary counselling is hampered by rivalries that seem more common
among prostate cancer specialists than in other cancer specialties. This must
change…. Close collaboration between surgeons, radiotherapists, and medical oncologists
is mandatory for substantially improved control of prostate cancer."
There
is no sign of any great change since that was written more than ten years ago.
In contrast to virtually every other cancer, where oncologists are directly involved
in the choice of appropriate treatment, prostate cancer is still mainly treated
by urologists, most of whom are surgeons. They will usually recommend surgery.
If a second opinion is sought from a radiologist, radiation therapy may well be
recommended for the same diagnosis. Both can quote statistics to support their
position - how can both be right? Until this is resolved, the newcomer to this
Strange Place must make up his own mind what is best for him and choose
a course of treatment balancing risks versus reward as defined by his values -
these generally include both survival and quality of life considerations. Hopefully
what follows will help him find his way through the uncertainty of this Desert
of Doubt.
|
MORE LANGUAGE HINTS
Before
moving onto the treatment choices it is important to understand that there are
no standard definitions for words like 'cured' or 'continent' or 'impotent' -
all very important issues in the decision making process.
Much
published information avoids stating definitions and outcomes directly and as
a result, men misunderstand the odds when choosing treatment.
To
make the decision that he will not regret, a man should understand his risk of
morbidity (side effects) as well as his likelihood of a "cure" and how these terms
are defined and measured.
|
When
asked, a doctor may present percentage figures or other data regarding the likelihood
of being 'cured', 'continent', and 'potent' following the course of treatment
being recommended. It is essential to make sure that the terms used are understood.
Most men expect 'cured' to mean that the tumour has been removed and that they
will have no sign of the disease again: they do not expect to have regular PSA
checks for the rest of their lives to ensure that the treatment has not failed.
They expect 'continent' to mean that they will not leak and will be able to urinate
without problems: they do not expect to have to use pads to remain dry or a penile
clamp to stop leaking. And they expect 'potent' to mean that they will be able
to achieve erections at will, whenever required: not to have to rely on medications
such as Viagra or injections or mechanical devices. Yet studies have definitions
of 'cured', 'continent', and 'potent' that differ markedly from these expectations
and actual outcomes of treatment may be worse than they are said to be because
of this. It is also important to understand that published information will usually
show the results achieved by very skilled and experienced practitioners. Their
results will almost certainly be better than someone who does not share these
traits.
Men should be free to decide that they would rather live with the
cancer than with the side effects of being treated for it. Men choosing treatment
should not expect to be free of its side effects; men choosing Active Surveillance
should expect eventual disease progression. These factors must be weighed against
a man's expected longevity and pre-treatment situation - for example many men
develop erectile problems as they age, so loss of this function might not be a
big issue for them; a man with severe urinary problems from BPH (Benign Prostate
Hyperplasia) might welcome the relief urinating freely again after surgery, and
accept the possibility of bit of leakage. A young man diagnosed with aggressive
disease is in a much different situation from that of an older man with low to
moderate risk disease. If the probability of the tumour having spread beyond the
gland is high, the odds of a 'cure' may be so low as to be a deciding factor not
to have aggressive treatment. Family history should also be considered: sharing
genes with someone gravely affected by prostate cancer may mean a genetic increase
the risks of not being treated.
As long as the death rate from prostate
cancer stays at about one in eight for those who have been diagnosed (regardless
of stage and grade), the decision not to have immediate treatment should not be
viewed as an illogical course.
TREATMENT
OPTIONS
Treatment options vary from country to country. The greatest
variety available is in the United States of America where, it is said, there
are at least fifteen, none of which are demonstrably better than each other. The
main options and sub-sets are:
 Surgery - This is the most common procedure, technically referred to as
RP (Radical Prostatectomy). The main sub-sets are "open" and "keyhole" or laparoscopic
procedures. Open surgery may be retropubic or perineal: keyhole surgery may be
manual or robotic. Men with advanced prostate cancer may have their testicles
removed surgically. This is called an Orchiectomy or an Orchidectomy, and although
a surgical procedure it is really a form of hormone treatment.
Surgery - This is the most common procedure, technically referred to as
RP (Radical Prostatectomy). The main sub-sets are "open" and "keyhole" or laparoscopic
procedures. Open surgery may be retropubic or perineal: keyhole surgery may be
manual or robotic. Men with advanced prostate cancer may have their testicles
removed surgically. This is called an Orchiectomy or an Orchidectomy, and although
a surgical procedure it is really a form of hormone treatment.
 Radiation Therapy - The most common form is EBRT (External Beam
Radiation Therapy) with a number of sub-sets that refer to the method of delivering
the radiation dose. Another form of radiation therapy - Brachytherapy -
has radioactive 'seeds' introduced into the prostate gland on a permanent or temporary
basis
Radiation Therapy - The most common form is EBRT (External Beam
Radiation Therapy) with a number of sub-sets that refer to the method of delivering
the radiation dose. Another form of radiation therapy - Brachytherapy -
has radioactive 'seeds' introduced into the prostate gland on a permanent or temporary
basis
 Androgen
Deprivation Therapy - This is referred to as ADT, but more commonly
known as Hormone Treatment. There are many variations on this type of treatment,
but essentially all involve using medication to suppress the hormonal mechanisms
that help tumours to grow. Orchiectomy, surgical removal of the testicles, is
an irreversible form of hormone treatment.
Androgen
Deprivation Therapy - This is referred to as ADT, but more commonly
known as Hormone Treatment. There are many variations on this type of treatment,
but essentially all involve using medication to suppress the hormonal mechanisms
that help tumours to grow. Orchiectomy, surgical removal of the testicles, is
an irreversible form of hormone treatment.
 Active Surveillance - AS is often referred to as "Watchful Waiting".
No conventional treatment is undertaken unless regular monitoring indicates disease
progression. Men choosing AS often make changes to diet and lifestyle with the
intention of boosting the immune system.
Active Surveillance - AS is often referred to as "Watchful Waiting".
No conventional treatment is undertaken unless regular monitoring indicates disease
progression. Men choosing AS often make changes to diet and lifestyle with the
intention of boosting the immune system.
 Cryotherapy - The prostate gland is frozen in this therapy usually referred
to as Cryo. The treatment is evolving and now includes focal cryotherapy aimed
at targeting a tumour (like a lumpectomy in breast cancer) and thus reducing the
probability of side effects. It is still regarded as somewhat experimental.
Cryotherapy - The prostate gland is frozen in this therapy usually referred
to as Cryo. The treatment is evolving and now includes focal cryotherapy aimed
at targeting a tumour (like a lumpectomy in breast cancer) and thus reducing the
probability of side effects. It is still regarded as somewhat experimental.
 High Intensity Focused Ultrasound- This procedure known as HIFU uses
the heat generated by the ultrasound to focus on and destroy the tumour. Developed
in China and used for some years in some European countries, Mexico and Canada,
it is still regarded as experimental in the United States of America.
High Intensity Focused Ultrasound- This procedure known as HIFU uses
the heat generated by the ultrasound to focus on and destroy the tumour. Developed
in China and used for some years in some European countries, Mexico and Canada,
it is still regarded as experimental in the United States of America.
 Chemotherapy - This treatment has not been used very much in dealing with
prostate cancer except as a last resort if all else fails. New chemicals and protocols
developed in the USA seem to be proving more effective than those in the past.
Chemotherapy - This treatment has not been used very much in dealing with
prostate cancer except as a last resort if all else fails. New chemicals and protocols
developed in the USA seem to be proving more effective than those in the past.
|
IMPORTANT INFORMATION REGARDING TREATMENT CHOICE
1.
Be certain that immediate treatment is required. Some leading experts in the
US say that the substantial majority of treatment procedures carried out for prostate
cancer in the US are unnecessary - estimates vary between 25% and 80%.
2.
The choice of treatment may be less important than the choice of who does the
procedure. The non-medical people in the prostate cancer community generally
agree the experience of the person or team carrying out the chosen procedure is
of utmost importance. The more experience, the less severe the side effects. This
may seem obvious, but many men only find out the hard way. It may be embarrassing
to ask a surgeon or radiologist to provide evidence of their skill, but bearing
in mind the consequences, this question should never be avoided.
3.
It is important to be as certain as possible that the disease is contained within
the prostate capsule before making any final treatment decision. This is where
the Partin Tables and other similar nomograms are very useful. The information
obtained by using the Partin Tables is no guarantee of the actual situation for
any individual. It does however provide some indication of what treatment options
might achieve the best result, and which might be ruled out because of the possible
extent of disease.
|
There
is need at this point for a short diversion to consider the tables before getting
back to the discussion of treatment choices.
Diversion
to consider the Partin Tables:
Allan W. Partin, M.D., Ph.D., and
Patrick C. Walsh, M.D. at the James Brady Urological Institute in Boston, USA
developed these tables which are based on the analysis of many biopsies. Their
aim was to try to establish if there was any relationship between the various
aspects of diagnosis and the likelihood of the disease having moved beyond the
capsule. The tables are too complex to reproduce in this document, but essentially
they look at the three main aspects of diagnosis - PSA (Prostate Specific Antigen),
Gleason Score and Clinical Staging - and show, as a percentage, the statistical
likelihood of the disease having escaped the capsule or being contained.
To
take the example referred to above, where the man was diagnosed as PSA 7.2: GS
3+2=5: Stage T2bNXM0, and referring to the relevant section of the Partin
Tables we would find the chances of:
o Organ-Confined Disease are Between
55% and 68% (median 62%)
o Established Capsular Penetration are Between 26%
and 38% (median 32%)
o Seminal Vesicle Involvement are Between 3% and 8% (median
5%)
o Lymph Node Involvement are Between 0% and 2%(median 1%)
To give
some idea of how one item might change these percentages, and how important the
Gleason Score is, if the diagnosis was PSA 7.2: GS 4+4=8: Stage T2bNXM0,
then the chances above would change to these:
o Organ-Confined Disease
Between 17% and 33% (median 24%)
o Established Capsular Penetration Between
29% and 48% (median 38%)
o Seminal Vesicle Involvement Between 16% and 39%
(median 27%)
o Lymph Node Involvement Between 3% and 20%(median 10%)
There
is a lower probability of benefit from surgery or other local treatments, if there
is a high probability of the disease having escaped from the organ.
Now,
back to treatment choices:
SURGERY: This
treatment is technically called RP (Radical Prostatectomy), and is often referred
to as the "gold standard" treatment, implying it is the very best. It is the treatment
most commonly prescribed for younger men or early stage prostate cancer. The traditional
surgery was an "open" procedure but there is enormous and rapid growth in laparoscopic-
'keyhole' - surgery, especially the Da Vinci robotic procedure.
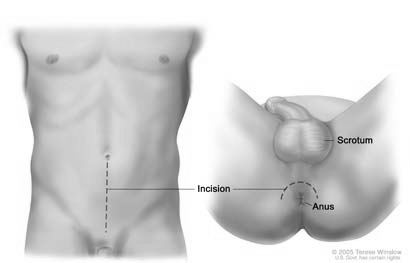
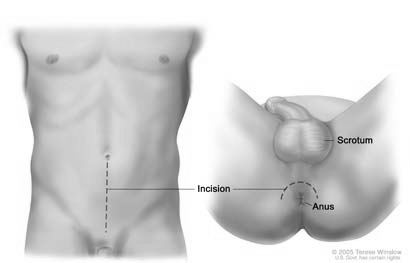
In open
surgery, the prostate gland is reached either from the lower part of the front
of the body - this is a retropubic procedure - or through the area between the anus and the
scrotum - this is a perineal procedure. There are no studies that show either
of these procedures to be superior to the other. In the past the operation involved
a substantial loss of blood. There have been significant improvements in surgical
techniques and it is now unusual for a transfusion to be required. Some surgeons
recommend the drawing and storing of the patient's own blood ahead of the operation
as a precautionary measure.
|
Retropubic Surgery
|
Perineal Surgery
|
Laparoscopic portholes
 Laparoscopic
surgery on the other hand requires five small ( five to 10 millimeters) incisions
(or portholes), one just above or below the belly button and two each on both
sides of the lower abdomen. Four arms are inserted into the portholes, three hold
instruments, the fourth holds the camera - this is the laparoscope which enables
the surgeon to get pictures of the prostate on a video monitor. Carbon dioxide
is passed into the abdominal cavity through a small tube placed into the incision
below the belly button. This gas lifts the abdominal wall to give the surgeon
a better view of the abdominal cavity once the laparoscope is in place. The arms
are used by the surgeon to remove the gland, through one of the portholes and
are manipulated manually, except where the procedure is robotic assisted - a procedure
usually referred to as the Da Vinci procedure. The surgeon sits at the console
and looks through two eye holes at a 3-D image of the procedure, meanwhile maneuvering
the arms with two foot pedals and two hand controllers. The Da Vinci System translates
the surgeon's hand movements into more precise micro-movements of the instrument.
Laparoscopic
surgery on the other hand requires five small ( five to 10 millimeters) incisions
(or portholes), one just above or below the belly button and two each on both
sides of the lower abdomen. Four arms are inserted into the portholes, three hold
instruments, the fourth holds the camera - this is the laparoscope which enables
the surgeon to get pictures of the prostate on a video monitor. Carbon dioxide
is passed into the abdominal cavity through a small tube placed into the incision
below the belly button. This gas lifts the abdominal wall to give the surgeon
a better view of the abdominal cavity once the laparoscope is in place. The arms
are used by the surgeon to remove the gland, through one of the portholes and
are manipulated manually, except where the procedure is robotic assisted - a procedure
usually referred to as the Da Vinci procedure. The surgeon sits at the console
and looks through two eye holes at a 3-D image of the procedure, meanwhile maneuvering
the arms with two foot pedals and two hand controllers. The Da Vinci System translates
the surgeon's hand movements into more precise micro-movements of the instrument.
RP,
whether open or laparoscopic is a major surgical procedure and will usually take
3 to 4 hours. Discharge from hospital was normally within 3 to 5 days for the 'open'
procedures but is now likely to be 3 or less. Laparoscopic surgery, on the other
hand, is far less traumatic and men are usually discharged from hospital in 24
hours. There is still a good deal of disagreement about the merits of the two
procedures. Surgeons favouring open surgery say that they can feel the prostate
and get a better idea of where the tumour might be and thus have more assurance
of negative margins: doctors favouring laparoscopic surgery say that the better
view obtained through the magnifying lens enables them to cut and stitch more
accurately. As yet there are no long term studies to support either view. The
incidence of initial morbidity are similar as are early failure rates. One thing
has become clear - the learning curve for the laparoscopic procedure is a long
one. One published study implies that it takes at least 250 procedures before
the surgeon can be regarded as proficient.
In
either case, a catheter will be in place, usually for some weeks. It normally
takes about three months to regain control of the bladder function, although some
men achieve this sooner. Recovery of erectile function will almost certainly take
a good deal longer, many months and sometimes a year or more. Recovery of erectile
function is dependent to a large extent on the ability of the surgeon to spare
the erectile nerves, although this is not the only factor.
The main benefit
of surgery is that it introduces an element of certainty. The prostate gland can
be examined closely to establish the extent of the tumour, to verify the Gleason
Score and to clarify the likelihood of the tumour being contained within the gland.
If there has been no spread beyond the gland, then the removal of the prostate
should, by definition, remove the tumour. For many men that is of utmost importance.
However,
surgery may not be a good choice if the disease has metastasised - that is if
the disease has spread to distant sites beyond the prostate. There is a view that,
in such cases, the removal of the gland and the main tumour may accelerate the
growth of the secondary, metastasised, tumours and make control of the disease
much more difficult. Like many other aspects of prostate cancer, there is no consensus
on this issue, which is the subject of some debate among physicians and researchers.
Because it is so difficult to establish beyond doubt whether the disease has spread
beyond the gland, there may be an element of risk in opting for surgery.
Success
or "cure" is measured by taking PSA tests at intervals after the surgery. Ideally
there should be no PSA measurement detectable with the normal PSA test. Ultra-sensitive
PSA tests may show very low levels - well below 0.10 ng/ml. No formal studies
have demonstrated the superiority of surgery over other forms of therapy, including
Active Surveillance, in early stage cancer. There is a failure rate of about 30%
- 35% over a period of 10 - 15 years for men undergoing surgery. Some failures
have been reported at 20 years. In the event of recurrence or failure of the treatment,
it is possible to use EBRT (External Beam Radiation Therapy) to treat recurrence
thought to be confined to the prostate bed, or to use ADT (Androgen Deprivation
Therapy) as a secondary treatment for recurrence where the disease has spread
into other areas of the body.
The main side effects of surgery are erectile
dysfunction (the difficulty or inability to have an erection) and bladder incontinence
(the inability to control the bladder). The man also becomes infertile, since
there is no ejaculate following the removal of the gland. Men intending to father
children should bank sperm before surgery.
The first of these problems
- erectile dysfunction (ED) - comes about because the nerves controlling erections
are embedded near the surface of the prostate gland; one on each side of it. There
has been a reduction in the reported rates of erectile dysfunction following the
development of what is referred to as the "nerve-sparing" technique and the use
of pharmaceutical drugs such as Cialis, Levitra or Viagra or one of the injectable
materials - MUSE, Tri-Mix and the like. However, the position of the tumour may
affect the ability of even the best surgeon to spare one or both of the nerves
while removing all the cancer. The ED rate is still high - probably over 50%,
especially for men over the age of 50. Studies quoted with better rates should
be examined very carefully, especially for definitions of potency or erectile
function. These studies usually involve excellent surgeons and may not reflect
the general outcome of surgeries carried out by surgeons with less experience.
Total
bladder incontinence is reported in a small number of men - about 5% - but many
men experience some leakage, particularly during sexual arousal or when lifting,
coughing, sneezing or laughing. Again it is important to look at definitions when
considering studies showing levels of continence after treatment. It is not uncommon
for the use of 'only' one or two pads a day to be regarded as fully continent
in such studies. The outcomes of surgery carried out by urologists who do not
have the experience of surgeons in a centre of excellence are usually worse.
Another
issue to be aware of is stricture from scar tissue, which can also cause urinary
problems. If the man has a history of poor scarring (some reports suggest that
if any scar on his body is more than 10 mm (about 3/8") wide) then there is about
an eightfold increase in urinary problems following RP (Radical Prostatectomy).
Penile shrinkage is also reported in a significant number of men, thought
to be the result of maintaining the penis in the flaccid state during what can
be many months of recovery of erectile function. It is thought this can be counteracted
by stimulating erections with drugs or manual devices as soon as post-surgical
healing has taken place.
A final issue, rarely discussed, is that of Peyronie's
Disease or Peyronie's Syndrome. This condition is one where the erect penis acquires
a 'bend' or deflection. The vast majority of Peyronie cases are very mild but
others can cause severe problems. It seems unlikely that the condition is directly
caused by a disease, or that it has any direct link with prostate cancer. A common
cause is thought to arise from accidents during sexual activities, especially
if the penis is not fully erect.
RADIATION
THERAPY - most common form of Radiation Therapy is known as EBRT (External
Beam Radiation Therapy). There are many other acronyms, such as RT (Radiation
Therapy), IMRT (Intensity Modulated Radiation Therapy) and 3DRT. All refer to
the procedure where photon radiation is directed at the site of the prostate gland
from an external source. The variations usually refer to the different aiming
techniques. A form of EBRT known as CyberKnife® delivers what are termed hypofractionated
doses - fewer doses, very much larger than normal EBRT but, it is claimed, delivered
more accurately and thus reducing the potential for collateral damage. A significantly
different form of EBRT is PBT (Proton Beam Therapy). It is claimed that the proton
beams can be directed more accurately than photon beams, again with less likelihood
of collateral damage. PBT for prostate cancer is only done at a few sites, mostly
in the US.
Another
form of radiotherapy, is Brachytherapy or SI (Seed Implants). Radioactive "seeds"
are implanted directly into the prostate gland, where they remain. There is a
variation of this treatment known as HDR (High Dose Rate Brachytherapy) where
seeds are inserted and then removed.
All
radiation therapy is intended to destroy the cancer cells while leaving healthy
tissue intact and is often the recommendation for older men for whom surgery presents
a health risk. EBRT is also used where it is felt that the tumour has spread beyond
the prostate gland and as a "salvage" treatment for failed surgery. EBRT used
in conjunction with other treatments such as surgery or brachytherapy is known
as adjuvant treatment. Radiation treatment is not recommended for men who have
a high International Prostate Symptom Score (IPSS) prior to treatment. This signals
severe urinary problems. Radiation therapies will often exacerbate these problems.
The International Prostate Symptom Score (IPSS) is generated from what is termed
a LUTS test (lower urinary tract symptoms).
EBRT takes place over a number
of weeks - usually six or seven - with daily sessions of therapy, the exception
being CyberKnife® which takes about five days. The effect of radiation is cumulative,
so low doses given on a regular basis build up into high doses, lethal to the
tumour cells. Most men tolerate the procedure very well, although as time goes
by, they may feel fatigued and it may be desirable to rest in the afternoon. The
feeling of fatigue will usually disappear after completion of the treatment.
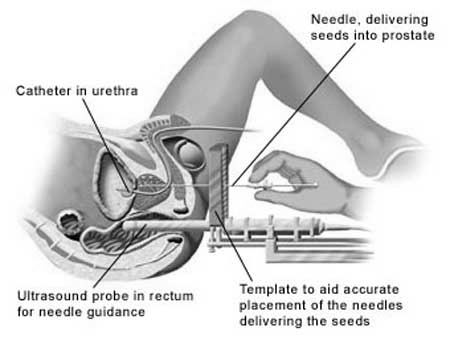 Illustration of placement of seeds into prostate in brachytherapy procedure
Illustration of placement of seeds into prostate in brachytherapy procedure
Brachytherapy
is usually considered as an alternative to surgery for men with a suitable diagnosis.
SI is a relatively short procedure, taking two or three hours, after which the
man can go home and carry on with his normal activities: HDR might need an overnight
stay in hospital. There is sometimes a feeling of fatigue, as is the case with
EBRT, but this usually recedes with time, as the dosage from the seeds reduces
(they are only fully active for about six months). Brachytherapy is not a good
option for a man who has previously had a TURP (Transurethral Resection of the
Prostate).
Two
aspects of SI could cause some concern. Firstly, the man is carrying radioactive
seeds in his prostate and the question asked is whether those seeds can injure
anyone close to the man - for example, grandchildren sitting on his lap. Studies
have demonstrated this is not a risk. The second point concerns seeds migrating
from the prostate to other parts of the body, notably the lungs. This happens
when seeds work their way out of the prostate before the glandular tissue heals
and locks them in place, or where they have not been securely placed. It is said
this does not present any significant problem for the patient.
Success
or "cure" for radiation treatments is measured by a gradual reduction in PSA level
in the months after treatment is completed. The aim is to achieve a nadir, or
low point, of 0.200 ng/ml and to maintain that level. Some authorities feel a
nadir of under 1.00 ng/ml is an acceptable level. Some men experience what is
referred to as a "bump" about 18 months after radiation when the PSA rises and
then falls again. No formal studies have demonstrated the superiority of radiation
therapy over other forms of therapy, including Active Surveillance. There is a
failure rate of about 30% - 35% over a period of 10 - 15 years for men undergoing
radiation therapy. A leading US institution claims better long-term freedom from
disease using combined SI/EBRT therapy rather than EBRT alone. They term this
treatment procedure as ProstRcision®.
In the event of recurrence or failure
of radiation treatment, surgery is not a good option and is rarely successful
because of the damage done to the tissue by the procedure. The usual option for
further management is ADT (Androgen Deprivation Therapy) although Cryotherapy
can also be used as a salvage treatment.
The side effects of radiation
therapy are similar to surgery with the added complication of urinary urgency/frequency,
difficulty in starting a urine stream and incontinence. Radiation can sometimes
result in bowel incontinence as well as rectal bleeding. ("Incontinence" is the
inability to control bladder or bowel). The reported incidence of bowel incontinence
is fairly low for EBRT and even lower for SI and PBT. There is a reported improvement
in radiation treatment side effects with modern techniques. Erectile dysfunction
is reported to occur in a substantial number of cases, more so for EBRT than SI,
but at about the same level as surgery. In contrast to surgery, where an immediate
loss of function can be followed by a gradual recovery, erectile dysfunction associated
with radiation therapy of any kind tends to occur well after treatment and to
gradually grow worse over time.
ADT (ANDROGEN
DEPRIVATION THERAPY) generally known as Hormone Treatment. There are
many variations of this treatment, all with different acronyms. The theory behind
this treatment is that growth of prostate cancer cells is fuelled by dihydrotesterone
(DHT) a derivative of testosterone, the male hormone steroid, which is an androgen.
A reduction in the production of androgen will therefore theoretically deprive
these cells of nutrition and they will die. There are four methods by which the
cells are deprived of androgen.
 Ablation. The testes produce approximately 90% of the male body's testosterone
with the balance being produced by the adrenal glands. Thus a simple way to reduce
testosterone production is the surgical removal of the testes by way of an orchiectomy
or orchidectomy (castration).
Ablation. The testes produce approximately 90% of the male body's testosterone
with the balance being produced by the adrenal glands. Thus a simple way to reduce
testosterone production is the surgical removal of the testes by way of an orchiectomy
or orchidectomy (castration).
 Additive. Testosterone production is attacked by dosing the man with oestrogen.
Additive. Testosterone production is attacked by dosing the man with oestrogen.
 Inhibitive.
This involves the use of chemicals to block signals from the brain to the production
centres so that no testosterone is produced.
Inhibitive.
This involves the use of chemicals to block signals from the brain to the production
centres so that no testosterone is produced.
 Competitive. The final method of treatment involves what are known as antiandrogens.
These do not prevent the production of testosterone, but block the receptors on
the prostate gland, preventing the androgen from being absorbed.
Competitive. The final method of treatment involves what are known as antiandrogens.
These do not prevent the production of testosterone, but block the receptors on
the prostate gland, preventing the androgen from being absorbed.
The last
three treatments are sometimes used in unison, in which case the treatment is
referred to as CHT (Combined Hormone Therapy) or ADT3. Treatment is administered
in a variety of forms, from pills to monthly or quarterly injections.
ADT
was at one time only used to manage late stage prostate cancer, where the tumour
had spread beyond the capsule and therefore could not be treated by surgery or
radiation and/or as a "salvage" therapy for failed surgery or radiation treatment.
There is however a growing use of this therapy as a precursor to other treatments.
This is known as neo-adjuvant therapy. Many practitioners are opposed to this
practice because studies do not show any significant advantage for the inevitable
side effects and there are several disadvantages. Some leading practitioners of
both surgery and brachytherapy in the US will not treat men who have had this
neo-adjuvant therapy.
The aim of ADT is to manage and control the disease,
since it is extremely unlikely that this therapy will result in a permanent "cure".
The degree of success achieved is measured by the reduction of the PSA to as low
a level as possible and keeping it there. In many cases the PSA level can be undetectable
and there are reports of men treated with this therapy achieving mortality rates
very similar to those of men without the disease. Failure of this treatment occurs
when the tumour becomes androgen independent (AI). This condition is often referred
to as AIPC - Androgen-Independent Prostate Cancer, or Hormone Refractory Prostate
Cancer (HRPC). This means the tumour has found a way of growing without the androgen
associated with testosterone. Management of the disease at such a stage is very
difficult although some success has been reported with new chemotherapy drugs.
There
are numerous side effects associated with this form of treatment whether the treatment
is being used as an adjuvant treatment for early stage tumours or as a palliative
measure for advanced cancers. Some men have severe side effects, others have
none: some appear early, some only after a long period of treatment. The ones
reported most frequently by men undergoing any of the ADT methods are erectile
dysfunction, loss of libido (no interest in sexual activity), hot flushes, osteoporosis
(loss of bone), loss of muscle tone, weight gain and mood swings, with depression
being widely reported.
Individual methods have other side effects such
as the development of breasts, increased risk of thrombosis, and an initial rise
in tumour activity, known as a "flare". This is usually of a temporary nature.
Flare can be prevented by administering an anti-androgen one week prior to the
first injection of the drug being used to inhibit testosterone production.
A
list of potential side effects associated with ADT include:
Alcohol intolerance
(with Casodex and Eulexin); Anaemia; Anxiety or depression; Arthritic symptoms;
Appetite loss; Blood in urine; Breast swelling and tenderness (gynecomastia);
Cholesterol and triglyceride increase; Constipation; Diarrhoea (eulexin); Disturbed
sleep; Drowsiness; Dry mouth; Emotional instability (esp. Crying); Feet or lower
legs, swelling of (peripheral oedema); Flatulence; Flu syndrome; Hair: decrease
in pubic and axillary hair; facial hair grows more slowly; Headache; High blood
pressure (hypertension); Hot flushes; Hyperglycaemia (high blood sugar ); Impotence
(during the period of treatment and some months after); Indigestion; Itching;
Insomnia; Liver problems; Memory loss; Methemoglobinemia (a crystallization in
the blood); Nausea; Nocturia (need to urinate frequently at night); Nervous and
twitchy legs; Osteoporosis; Pain: abdominal, back, chest, in right side; Pressure:
feeling of extreme pressure in head; Prickling sensation on the skin; Shortness
of breath; Testicular atrophy (shrinking) & soreness; Sweating; Weight gain (weight
gain may continue for a while after treatment); Weight loss.
|
SERIOUS
ADT SIDE EFFECTS
The
following symptoms may reflect serious problems and if they occur, medical attention
should be sought immediately:
Bluish lips, fingernails, or palms of hands;
Dizziness (extreme) or fainting; Fatigue, weakness; Pain: bone, joints, pelvic;
Numbness, coldness, or tingling of hands or feet; Infections; Rash; Urinary incontinence;
Urinary tract infection; Vomiting; Weak and fast heartbeat; Yellow eyes or skin.
|
A
recent development has been towards "pulse" therapy known as IHT (Intermittent
Hormone Treatment) or IHB (Intermittent Hormone Blockade). Some studies indicate
that stopping the ADT once the PSA count has been reduced and reintroducing the
therapy if the PSA count rises again might produce some benefit. The duration
of the side effects of ADT are reduced and it appears the possibility of the disease
becoming androgen-independent may also be lessened. In some very rare cases, the
PSA does not rise again after the ADT is stopped and the man can be considered
to be in remission. Men on ADT welcome the treatment "holidays" as many of the
side effects disappear or diminish as the effect of the drugs wears off. In some
cases some of the side effects are permanent.
CRYOTHERAPY:
This procedure uses probes to freeze the gland. The prostate tissue is destroyed
by the very rapid thawing process which ruptures the cell membranes. The probes
are placed through the perineal skin - between the scrotum and anus, like the
tubes for brachytherapy. They are guided using transrectal ultrasound which is
also used to monitor the freezing process in real time. It is unusual for fewer
than three probes to be placed; additional probes may be placed to allow for adequate
freezing of more extensive disease. Incontinence levels are kept low by warm liquid
being circulated in the urethra during the procedure.
When this procedure
was first used, the entire gland was destroyed, which led to a very high incidence
of erectile dysfunction - almost 100% of men were impotent according to some studies.
Later developments have seen the development of focused cryotherapy, which destroys
only identified tumours and the healthy cells in the immediate vicinity of the
tumour, leaving some or all of the erectile nerves untouched and resulting in
levels of ED that are comparable with those resulting from other treatments. It
can be difficult to pinpoint the position of small tumours. This usually involved
a mapping biopsy using a large number of needles - as a rule of thumb the volume
of the gland + 20 up to a potential maximum of 100 needles. This type of biopsy
is usually undertaken under a general anaesthetic. .
One advantage this
form of treatment has is that it can be repeated and it can be used in suitable
cases as a salvage procedure for other failed treatments, notably radiation.
HIGH
INTENSITY FOCUSED ULTRASOUND (HIFU): This procedure was developed in China
and used for liver and pancreatic cancers, but was not used initially for prostate
cancer. Subsequently several European countries, notable, France, Germany and
Belgium started to treat men with prostate cancer. Basically the tumors are cooked
to death quickly. The focused sound energy raises the temperature to around 140
degrees Fahrenheit (60 degrees Celsius), killing the cells in about one second.
The ultrasound beam must travel through continuous tissue or fluid to the tumor
site because the energy cannot be focused through gas or bone. By targeting tumour
cells precisely, theoretically the tumor can be destroyed with minimum collateral
damage. Like cryotherapy one of the immediate pre-treatment issues is how to identify
the precise location of the cancerous cells.
HIFU is still regarded as
experimental in a number of countries and has not been approved for prostate cancer
by the FDA in the USA. Trials are being carried out there.
There
have been alarming reports of bladder damage creating severe urinary problems.
It is clear that experience with the equipment used for this therapy is even more
important than in other therapies. An unskilled practitioner can do a deal of
damage very quickly.
ACTIVE SURVEILLANCE:
This option is still often referred to as WW (Watchful Waiting) although the terms
have different meanings. In the past Watchful Waiting meant no action was undertaken
unless the disease is seen to progress. Men choosing the Active Surveillance are
monitored closely and will often use a variety of non-conventional or alternative
treatments to manage the progression of the disease.
Dr.
Jon Oppenheimer, a leading pathologist in the USA is on record as saying:
"For
the vast majority of men with a recent diagnosis of prostate cancer the most important
question is not what treatment is needed, but whether any treatment at all is
required. Active surveillance is the logical choice for most men (and the families
that love them) to make."
|
The
rationale for this statement is that prostate cancer is what is termed an "indolent"
disease in most cases, because it progresses so slowly it may never be a threat
to life. The man choosing Active Surveillance over Watchful Waiting believes by
taking a proactive stance he can harness his immune system to either halt the
progress of the disease or possibly even cause it to regress.
Prime
candidates for this option are those who have been diagnosed with an insignificant
tumour or very low risk disease. There are various definitions of these terms,
but broadly speaking they are similar to the one established by Johns Hopkins
University School of Medicine in the US, where the definition of an insignificant
tumour was established some years as one with the following characteristics:
 Nonpalpable - the examining doctor would not feel anything when carrying
out the DRE (Digital Rectal Examination)
Nonpalpable - the examining doctor would not feel anything when carrying
out the DRE (Digital Rectal Examination)
 Stage T1c - the tumour is discovered in the course of a biopsy following
an elevated PSA test where there are no other symptoms
Stage T1c - the tumour is discovered in the course of a biopsy following
an elevated PSA test where there are no other symptoms
 Free PSA - the percentage of free PSA should be 15% or greater
Free PSA - the percentage of free PSA should be 15% or greater
 Gleason Score - less than 3+4=7 - or, as some practitioners have it, 7 or
less
Gleason Score - less than 3+4=7 - or, as some practitioners have it, 7 or
less
 Size - less than three needle cores positive with none greater than 50%
tumour. (In this definition it is assumed that a 12 needle biopsy is used)
Size - less than three needle cores positive with none greater than 50%
tumour. (In this definition it is assumed that a 12 needle biopsy is used)
The
latest guidelines issued by National Comprehensive Cancer Network (NCCN®) following
the codified changes to the Gleason grading system in January 2009 has this definition
of very low risk disease:
 Clinical Stage T1-T2a - the examining doctor felt nothing on DRE or felt
something on one side of the gland only
Clinical Stage T1-T2a - the examining doctor felt nothing on DRE or felt
something on one side of the gland only
 Gleason Score 6 - the lowest score on the current range
Gleason Score 6 - the lowest score on the current range
 PSA less than 10 ng/ml
PSA less than 10 ng/ml
 Size - 3 positive needles or less with 50% or less positive material in each
core
Size - 3 positive needles or less with 50% or less positive material in each
core
 PSA density - less than 0.15 ng/ml/gm
PSA density - less than 0.15 ng/ml/gm
Old
studies have shown the majority of men with such a diagnosis will not have a life-threatening
progression of the disease for many years. Current studies demonstrate that there
is a negligible risk for suitable men in undertaking Active Surveillance.
The
precise protocols for men choosing Active Surveillance vary, but broadly speaking
they involve regular PSA tests (every man diagnosed with prostate cancer will
continue to have these tests for the rest of his life to monitor him for any progression
or return of the cancer) and other tests, notably biopsy procedures and DRE (Digital
Rectal Examinations). Initially these may be done annually, but there is a view
that once it has been established that the disease shows no sign of progression,
the period between procedures may be extended. Other tests and scans, such as
Color Doppler scans may be used to monitor significant changes in the tumour.
Because
men choosing Active Surveillance have still have an untreated, entire gland they
may therefore have to deal with issues such as BPH (Benign Prostate Hyperplasia)
- the enlargement of the gland which causes urinary problems. BPH can be successfully
managed with a variety of drugs or procedures such as a TURP (Trans Urethral Resection
of the Prostate) - often referred to as a 'rotor rooter' operation .
The
problem for any man considering Active Surveillance is the uncertainty of the
diagnostic process, which is more art than science. It is not possible to identify,
with absolute certainty, which tumours are indolent (the kitty cats) and which
are aggressive (the tigers) or just where they fit in the range of diseases. There
are good indicators: The ones listed above indicate disease that is most likely
indolent; on the other hand PSA doubling times measure in months or weeks, high
Gleason Scores - over 20 ng/ml, late stage disease - stages T3 and T4 all indicate
a disease that requires early attention. Indolent disease can often be treated
like a chronic illness.
For
many men choosing this course, the essence of Active Surveillance is a belief
in the mind/body continuum. The aim is to maintain the immune system in good condition
to deal with the tumour. Since there are very few studies to guide men in this
endeavour, and the medical professionals are often ill-informed on nutritional
matters and similar issues, there is a tendency for each man to develop his own
unique program. Most of the programs for which there is anecdotal support include
the following elements:
 Stress reduction: Stress is commonly regarded as one of the most
universal causes of damage to the immune system. Stress reduction can be accomplished
using activities such as meditation, visualisation or yoga.
Stress reduction: Stress is commonly regarded as one of the most
universal causes of damage to the immune system. Stress reduction can be accomplished
using activities such as meditation, visualisation or yoga.
 Exercise: Moderate amounts of exercise are essential. Usually, subject
to the fitness of the man, he is recommended to exercise at least three days a
week at a level where the pulse rate is raised and sweat is formed.
Exercise: Moderate amounts of exercise are essential. Usually, subject
to the fitness of the man, he is recommended to exercise at least three days a
week at a level where the pulse rate is raised and sweat is formed.
 Changes in diet: This subject is covered in a little more depth
in the section titled Plains of Recovery, but essentially, the aim is to
attain a vegetarian diet or better still a vegan diet. Red meat and dairy products
are regarded as bad: fresh vegetables and fruit are regarded as good. Smoking
should, of course, be stopped, as should consumption of alcohol, although small
quantities of wine, especially red wine, are thought to be beneficial. Consumption
of coffee, animal fats, fried foods and sugar should be kept to a minimum.
Changes in diet: This subject is covered in a little more depth
in the section titled Plains of Recovery, but essentially, the aim is to
attain a vegetarian diet or better still a vegan diet. Red meat and dairy products
are regarded as bad: fresh vegetables and fruit are regarded as good. Smoking
should, of course, be stopped, as should consumption of alcohol, although small
quantities of wine, especially red wine, are thought to be beneficial. Consumption
of coffee, animal fats, fried foods and sugar should be kept to a minimum.
 Weight loss: There is a clear connection between illness and obesity.
Although following the steps above should lead to weight loss, this should also
be incorporated as one of the aims of any successful program.
Weight loss: There is a clear connection between illness and obesity.
Although following the steps above should lead to weight loss, this should also
be incorporated as one of the aims of any successful program.
Successful
Active Surveillance management should see a stabilising or even a reduction in
PSA levels, and this is the primary measure of success. Because of the vagaries
of PSA counts, this should not however be the only measure. There should also
be an annual DRE (Digital Rectal Examination) and, some recommend, an annual or
biennial biopsy. In considering this latter test, some thought should always be
given to the potential for side effects from biopsy. A continuous rise in PSA
or a positive DRE would be the trigger to contemplate further, conventional treatment.
Many men - more than 20% in one study - who have chosen Active Surveillance have
negative biopsy results on repeat biopsy. This does not necessarily mean that
there are no longer cancer cells in the gland, because the biopsy process is literally
'hit and miss' but it does imply that there has been little or no significant
growth in the tumour.
The side effects of a successful Active Surveillance
program are all positive since the enhanced immune system will generally result
in better health all round.
It is often difficult to deal with the uncertainty
associated with Active Surveillance. This is often seen to be greater than the
uncertainty of those who have had conventional treatment. However in three studies
it has been found that essentially, if men are 'worriers' they have similar levels
of concern whatever the path they choose. Those who are more phlegmatic accept
the uncertainty more easily.
Anyone
embarking on Active Surveillance will need determination to continue. The medical
profession along with well-meaning friends and relatives, often create a good
deal of pressure to 'do something'. This leads many men to abandon Active Surveillance
and opt for conventional treatment even if there is no significant change in the
diagnostic pointers.
|
Back to top
GO
NOW to Part 4 - Beyond Treatment - The Plains of Recovery



 Laparoscopic
surgery on the other hand requires five small ( five to 10 millimeters) incisions
(or portholes), one just above or below the belly button and two each on both
sides of the lower abdomen. Four arms are inserted into the portholes, three hold
instruments, the fourth holds the camera - this is the laparoscope which enables
the surgeon to get pictures of the prostate on a video monitor. Carbon dioxide
is passed into the abdominal cavity through a small tube placed into the incision
below the belly button. This gas lifts the abdominal wall to give the surgeon
a better view of the abdominal cavity once the laparoscope is in place. The arms
are used by the surgeon to remove the gland, through one of the portholes and
are manipulated manually, except where the procedure is robotic assisted - a procedure
usually referred to as the Da Vinci procedure. The surgeon sits at the console
and looks through two eye holes at a 3-D image of the procedure, meanwhile maneuvering
the arms with two foot pedals and two hand controllers. The Da Vinci System translates
the surgeon's hand movements into more precise micro-movements of the instrument.
Laparoscopic
surgery on the other hand requires five small ( five to 10 millimeters) incisions
(or portholes), one just above or below the belly button and two each on both
sides of the lower abdomen. Four arms are inserted into the portholes, three hold
instruments, the fourth holds the camera - this is the laparoscope which enables
the surgeon to get pictures of the prostate on a video monitor. Carbon dioxide
is passed into the abdominal cavity through a small tube placed into the incision
below the belly button. This gas lifts the abdominal wall to give the surgeon
a better view of the abdominal cavity once the laparoscope is in place. The arms
are used by the surgeon to remove the gland, through one of the portholes and
are manipulated manually, except where the procedure is robotic assisted - a procedure
usually referred to as the Da Vinci procedure. The surgeon sits at the console
and looks through two eye holes at a 3-D image of the procedure, meanwhile maneuvering
the arms with two foot pedals and two hand controllers. The Da Vinci System translates
the surgeon's hand movements into more precise micro-movements of the instrument.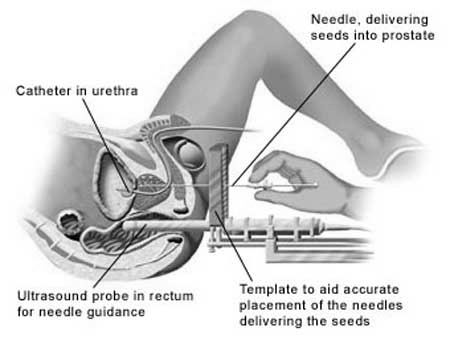 Illustration of placement of seeds into prostate in brachytherapy procedure
Illustration of placement of seeds into prostate in brachytherapy procedure