THERE WAS NO RESPONSE TO AN UPDATE REMINDER IN 2021 SO THERE IS NO UPDATE.
I have resisted having a PSA test but have had some waterworks problems for around 10 years (sudden urges, dribbles). GP added PSA to a recent blood test and came back 10.0 ng/ml - Saw a urologist and had an 18 point biopsy - Never again! Had to have the next day off work but no infections.
I don't think much of any of the treatment options but have read a lot of good info. I have made big changes to diet and am doing meditation, imaging and so on. I believe my own immune system is my best bet for a cure. All I need to do is get those killer T cells to recognise cells that express PSA. My brother was recently diagnosed as well. I will let him know about YANA - I am so glad I found this website. Thanks for being here. More news later.
I have changed my diet to include more selenium, omega 3, green tea, fruit and veg. I have reduced red meats and cut out sugar and reduced fats. By November 08 my PSA had risen to 11 (from 10 in July) and in Feb 09 it was 12. I wonder why I just get whole numbers and do they round it off to whole numbers? My uro says it just happens my PSA is what it is. Anyway both GP and uro are now saying its time to do something about it. Things are tense at home as the fear of an uncertain outcome hangs over our heads. I have now retired and am driving my wife nuts as we make the change to seeing more of each other.
I am still undecided about treatment but afraid if I do nothing and the numbers keep rising I may have left it too late. There is a lot of conflicting information, advice and opinion around. My brother has opted for surgery in April. I am leaning towards EBRT at this time but radical surgery would be quicker. I have ruled out brachytherapy. Uro says there is nothing to pick between the two but he is a rather clinical b... I told him I still have painful orgasms 6 months after the biopsy and all he said was it should be better by now. I wonder if he nicked a nerve or something. Maybe he figured it doesn't matter as this guy will probably have it removed soon. I guess at the end of the day you take your chances and accept what comes.
I retired at the end of January and a week later found I have an inguinal hernia. Doctor says 'so what'. it might be a common condition but still a worry.
Anyway - next step is to decide on treatment. I asked for an appt with the radiologist to discuss options and opinions.
Will post more in next update.
By April 2009 my PSA rose to 12.0, 2 points in 6 months. GP said its time to make a treatment decision and I must admit I too was worried as the rise was more than I expected. I saw a radiation oncologist and commenced on Zoladex for three months.
By July my PSA fell to 1.0 and I was very pleased with this. The hot flashes were a bit of a problem and my libido fell to zero. Then I had the second Zoladex shot. After considering the side effects of radiation and the need to drive to the hospital every week day for two months, I made an appointment with a GP in Brisbane, 800km from home. I knew this GP from my previous job and respected his judgement and opinions. He referred me to a Urologist also in Brisbane. This Uro recommended surgery and advised he could perform an RP in a public hospital (PA). That was in October.
Why surgery? Briefly my reasons are - WW and diet changes did not stop the rise in PSA. Zoladex reduces PSA but cannot be used long term without unwanted side effects. No libido and no sexual response was changing who I am and was having a negative effect on our relationship. The side effects of radiation followed by the uncertainty of a complete cure was a worry. While RP is not ideal, my surgeon has had some excellent results with minimal leakage and is experienced in nerve sparing technique. He did warn that it may not be possible if the PC is too advanced. At the assessment appt, Dr M arranged to meet Lyn and I for his last appt and spent a long time examining my biopsy results and films and explained the pros and cons in great detail. We later did some research and discovered that Dr M is a leading surgeon and has pioneered some new techniques. While he normally operates in private hospitals he advised that he can operate in a large public hospital in Brisbane. I had been admitted to this hospital once before and feel very confident with the hospital and staff and especially with my uro. Much different to my earlier experiences.
So, feeling confident that this is the way to go, I am booked for surgery on Thursday 19th November. My brother also had his surgery there in April and is going well, although he had a different doctor.
Thanks to all the people who have emailed their support and best wishes to those undergoing treatment.
More news after the surgery.
Les.
Later: November 25 2009 I finally feel up to updating my story. I had surgery as planned last Thursday. The nurses were very supportive as they wheeled me to theatre, asked who I was, dob, etc a dozen times and the next thing I knew I was feeling very groggy in a room full of faces and people asking questions. All I wanted to do was go back to oblivion. I had not slept for 2 days prior to surgery and Lyn and I had driven 800km 2 days before hand. They took me up to the ward where I saw my beloved wife's face anxiously waiting. It was 6 hours since she last saw me. I did not sleep that night as I had tubes for drips, a catheter and was checked every hour or so. I also had two spare tubes in case the first one got blocked.
Next day the physio came to teach me how to breathe and get me on my feet. I did not feel ready but they got me up anyway. I had stockings on and things pumping my legs to aid circulation. They were removed and we went for a walk around the ward corridors using a walking frame. After one lap I said I couldn't do any more so it was off for a shower.
Me naked apart from my tubes, blood all round my 'old fella' and a great tube sticking out through it. Two nurses gave me a wash down. I was beyond embarrassment and I felt safe with them (emotionally). After that I felt dizzy and next thing passed out. When I came to there were people everywhere. A doctor checked me over and a nurse said I had been out for 5 minutes. Back to bed and begin to recover.
A few words on recovery; The day of surgery I could not keep my eyes open and the room felt very glary. I asked for the lights out and blinds closed. I did not sleep that night. Pain was OK due to on demand pain control.
Second day I felt good about surgery, everyone was positive and told me it went well. I saw the registrar who said I had a tiny prostate due to Zoladex. I was his first patient who had been on Zoladex prior to surgery. I felt positive and ready to try to get mobile. The catheter was not as bad as expected and the abdomen wound felt OK. I could not sit up without help. I had a bit of pureed porridge and fruit for breakfast. Drinking lots of water. I had not opened my bowels for two days and felt the need to go. The nurses helped me to the toilet but nothing doing. It hurt like hell and blood came from around the catheter. One nurse said it would come when ready and try to ignore it.
Did not sleep that night either. I had pain in my shoulder and chest and was very aware of my body. I could hear my heart beating all night, very disturbing. Next day I felt like crap, depressed, sorry for myself and wishing I had not had surgery. Later that day Lyn visited and insisted I watch TV. I didn't feel like doing anything, but there was a very interesting doco on Foxtel that got my attention off myself and after an hour I was feeling better.
By afternoon I was back on track. It appears that the day after surgery you may feel OK due to adrenaline and relief that it is over. Next day, shock sets in and you feel rotten and loss of hope. Getting my mind off the condition was the best thing. With Lyn's support and a return of appetite I started to improve.
I was discharged after 4 days and am now with Lyn at a nearby motel. I go back on 30th to have the catheter removed. Feeling much better and glad I did it.
Lyn is an angel and is putting up with much. It is a shame the hospital did not give her more support. She was not given any advice or comfort while waiting for me to return from surgery. People generally acted as if she was not there. I cannot complain about my treatment, but it would have been good if she had been included as part of the team. She is now supporting me and caring for me and herself without any help.
My thanks to mentors who have emailed their support and advice and especially to Joe Hodge who rang me twice in the hospital to encourage me. Thanks to Terry and all at YANA. Sorry for long winded update- more later. Keep up the fight against PCa. Life is for living.
It is 7 weeks post surgery and I have recently returned from a follow up visit to the hospital.
The good news: Surgery is healing very well, no blood in urine, continence 99% but still wear pads just in case. Doctor say he was able to spare both erectile nerves but no joy yet. I think I am still suffering effects of Zoladex, hot flashes and no libido to speak of. I am feeling positive and well. My strength is returning and I am quite active.
The not so good news: There were two positive margins on examination of prostate and involvement of left seminal vesicle. The tumour was 25% of the gland. Doc has referred me to a radiation oncologist in 3 months.
The dilemma: They are not sure if cancer cells are still present or not. PSA at 4 weeks was >0.03. PSA will be monitored prior to seeing RO. I am wondering if radiation may do more harm than good at this stage, especially if PSA drops to a lower level. Should I put off RT and monitor PSA for a while? At what point would RT become worthwhile?
Meanwhile life goes on and it is still worth pursuing goals.
Thanks to all at YANA for your support and best wishes to all fellow sufferers and their families.
Later: Lyn and I drove to Brisbane to see the radiation oncologist. Latest advice is that because of 2 positive margins and involvement of one seminal vesicle, I should undergo a further six weeks of radio therapy, just in case. Alternatively I could participate in a clinical trial where I would be assigned to either a group watching their PSA or a group receiving 60 greys of radiation.
The side effects of radiation were described. None good. However no one could tell me what would happen if I decide to have no further treatment. It comes down to a toss of a coin. Given that so far I have lost so much of my quality of life to Zoladex and surgery, I am leaning heavily to returning to Watchful Waiting and we will see what happens next.
Actually, I am very pleased because my latest PSA was undetectable, which has to be a good sign. If it remains undetectable I reckon I can say I am cured and if not, lets deal with it when the time comes. Next PSA in April, til then life is for living!!
Thanks again to all YANA contributors for your support and good wishes.
My PSA is rising after surgery and now 0.44. Seeing a Uro soon and hope to provide a complete update then.
Thanks and regards,
Les
I have just returned from getting my latest PSA. It is now 1.29. Doesn't sound too bad does it? Problem is, it is now almost tripling every two months!
In October 2010 it became detectable post surgery at 0.05. January was 0.15 March was 0.44 and now 1.29. I believe I am eating the right things, getting exercise, drinking green tea and trying to stay positive.
I am seeing a new urologist on Monday 30 May. If anyone can offer any suggestions, so I can at least ask some intelligent questions, I would be grateful.
Thanks again to everone for your support.
It's been an interesting year. In 2011 I went through the preparation for adjuvant radiotherapy as my PSA was rising. Rising? It was doubling every 5 weeks and I was getting a bi panicky about it. I have heard that some PCas are Tigers. Iwas convinced I had the daddy of the Bengals. Yet, Lyn and I both felt uneasy about RT. By July 2011 PSA was up to 3.1.(from 1.4 in May). Surgery had left some side effects, impotency but thankfully very minor incontinence. Extra problems due to radiation did not seem worth it, especially since they could not actually pinpoint any tumour. At the last minute my rad. onc. sent me for an MRI and identified a suspect lymph node.
We agreed to try Zoladex again, however it was suggested to wait a while. By Feb 2012 PSA; was 16 so started on 3 monthly Zoladex implants. March reading was 4.5 and May is 0.1. Maybe the tiger is just a pussycat!!
Side effects are just hot flashes and night sweats. Not too bad in winter, but I have to throw off the blankets. Uro has prescribed Androcur 25mg per day. Feeling a bit wary about added side effects, but think it may be worth a go. Uro wants me to stay on Zoladex for a year and if PSA stays below 1, may have a break. I handle hot flashes by thinking about how those ca cells are suffering!!! ("die you little buggers!!")
Thats it for now. Best wishes to all fellow sufferers. Meanwhile, life is for living, so visiting the family, camping, sailing and motorhoming are on the agenda.
Its been a while since my last update and things seem to be going pretty well. My PSA has dropped to undetectable. I want to stop the Zoladex treatment but my URO wants me to stay on it until May next year. He says he would like to see if it stays low for 12 months and then go intermittent. That's OK but Zoladex affects other areas of life as well. After about 6 months I began to experience what I call 'feelings of impending doom' at night when trying to get to sleep. This is always just before a hot flash. ('Flash' is not quite right, they last several minutes with a lot of sweating, throwing off blankets and clothing, often followed by feeling cold.) Hard to explain, but I guess it is kind of like a panic attack. The uro prescribed Androcur, but when I read the fine print. I was horrified. Bad enough on Zoladex, loss of libido, feeling nothing like my 'normal' self. Androcur sounded like it would just about finish everything else off as well. My wife suggested anti-anxiety meds. Spoke to my GP and he gave me 25 mg Dothep at night. Works a treat and no side effects to worry about. My wife still says I am not 'myself' and that is just something we have to cope with as best we can. I know she is right, but that is the nature of this Pca and its consequences. Better than the alternative though!!
That's about all my news - changed email some while ago so apologies to anyone who has tried to contact me.
God bless all of us sufferers.
Not much to tell at the moment - just waiting on next PSA and due to see uro next month. No real changes since last update except did not have Zoladex implant in May. It's just wait and see. I am feeling good, doing a bit of work and saving for another cruise. Went on an 11 day cruise in March, first time- It was GREAT!! My advice - Do something you have always wanted to do but kept putting off.
It is now 9 months since my last Zoladex implant. PSA was 0.08 in July and 0.8 a week ago. While I am naturally concerned about this rise it is too early to panic so I will wait and see if the rate of increase improves. I plan to monitor at 6 week intervals for a while. On the good side, some small improvement in EF (erectile function). Could be some nerve regeneration but too early to say. Has anyone tried "Black Salve"? I read a bit about it and saw some results on a video. I am thinking about giving it a try internally, starting very small and see if any effect on PSA. I may as well be my own guinea pig! The medical options don't seem to hold any better prospects. Will keep you posted.
Best wishes to all fellow sufferers and your families.
Les
Can't believe it's over a year since my last update, apologies for that. Let's get the bad news out of the way first. Around March my PSA started to rise- by June/July it was doubling every 4 weeks. Saw my uro in August and decided to go back on Zoladex 3 month implants when PSA estimated to reach around 20.
Mid September it was back for the big needle- my GP is gentle and anaeshetises my belly before she does the implant.
The good news - Last PSA early November was 1.35 so looks like Zoladex is still effective. I expect it will fall further. Otherwise health is not too bad for a 67 year old. I am back at work for 6 months for a stint as a part time employee. Looking forward to a cruise in February.
PCa does not dominate my thoughts any more. I often go for days without even thinking about it. I still have some confidence that a more effective treatment will be found before too long. On the other hand, the way the world is going, an early exit might not be so bad (just kidding!!)
Best wishes to all fellow sufferers and your families.
Les
Early 2015 my PSA was around 1.7 and I started taking Casudex tablets daily. By July PSA had risen to 3.4.
In December PSA had risen to 11.7. I now see only my radiation oncologist as he is better equipped to monitor progress and I don't plan to have surgery anytime soon. I have now stopped Casudex and continuing Zoladex. I have been referred for a psma scan. This is fairly new technology and can see very small metastases. This should happen this month.
I will post an update after I see the scan results. Meanwhile I feel good and have no physical symptoms of pca.
Best wishes to all readers.
Les
Last PSA was a bit of a shock, up to 22.9. Rad Onc referred me for a psma scan, very interesting day, no discomfort. They gave me a CD-ROM to take home. Clearly shows a bright spot in left hip area. I have noticed some pain in that area that I put down to back strain. Felt worse after I saw the scan! Psychosomatic?
Now I am to have 6 shots of radiation to left hip starting March 4. No other mets seen so that is something to be thankful for. Not sure if radiation is the best way to go but don't have many other choices so we will give it a bash and see what happens.
Best wishes to all
Les
End of Feb, PSA up to 29.2 pre radiation. Mar 4 commenced 6 sessions of radiation, 5 greys per session. I did not experience any skin burning, however hip has felt weak ever since. I tire easily and walking is no fun due to discomfort in my hip.
I am due to see my rad onco next week. Just have to wait and see. Meanwhile I am taking a mix of bicarb soda and maple syrup. Google for details. It is supposed to kill cancer cells. Hit em while they are down I say. Anything worth a try. Don't fancy having chemo though. Will update after seeing onco.
Best wishes to all.
Les
I visited my onco two weeks ago. PSA has dropped to 11.2. Hopefully will continue dropping. I did not realise how weak I have become until I put a new clutch in my daughter's car a few weeks ago. Took me two days and after that I was buggered. My hip is feeling better and I can walk a couple hundred metres now. I did some research into the bicarb maple syrup thing and it confirms my suspicion that all gets broken down long before any sugars reach the cancer cells. By the way, my onco says I probably have millions of them floating around even though they can't see them. Do something you enjoy he says.
Next PSA is in three weeks and I see the onco again. Will update story soon.
God bless all of us living this nightmare.
Best wishes to all sufferers and your families.
Les
I visited my radiation oncologist today, PSA is down to 8.0. My weight has only dropped 1.5kg. RO is pleased with results and will see me again in 4 months. I am to continue on Zoladex as he believes most of the pc cells are still responding to treatment. I will check PSA with my gp in 2 months. So far a good result and worthy of a celebration. Thank you to all of you who are supporting me with your good wishes.
God bless all of us sufferers and our loved ones.
Les
Latest PSA today is down to 5.03 from 8.0 6 weeks ago. No lasting side effects apart from tired and weight loss. I have lost 5.5 kg this year. It could be due to other factors as l have reduced appetite. I am having a gastroscopy and colonoscopy tomorrow to investigate.
Meanwhile, all smiles.
Thank you to all my supporters.
God bless all fellow sufferers.
Les
Since my last update I have moved to Canada. The details are not really suitable for these pages.
Today I received my latest PSA and it is down to 3.4 and it appears it will continue to fall. The change has meant that I no longer have access to the wonderful health care system provided in Australia. However I have been happier since moving and I feel this has improved my overall health. I brought a 3 month Zoladex 10.8 depot with me from Australia. It would normally be due around now, however I have decided to save it for when and if the PSA begins to rise again. The cost of doctors and medications is very high here and my insurance won't cover a pre-existing condition. I plan to continue the maple syrup/baking powder as it is not doing any harm and may well be doing good. I plan also to try black salve internally. Has been tried by others without ill effects.
So, today I am very happy and feel cause to celebrate!!
Best wishes to all fellow sufferers, life is for living, so live while you can!!
Les
With some trepidation I have decided to commence taking black salve, also known as cansema, internally. This treatment is not supported by the medical fraternity so it is well to note that I take it at my own risk. Those who may be interested can learn more by researching the internet. I plan to take one dose (about the size of a pea) daily for 10 days, then stop for ten days and repeat until I have taken 30 doses. I will then check my PSA.
I started by loading gel capsules with a dose measured by a plastic syringe. Next day, the black salve had dissolved the capsules, making a bit of a mess. Not such a good idea. It would probably be ok if the capsules were taken soon after filling. However, I took the salve with a piece of bread and followed by a good meal. It tastes a little bitter but no ill effects after 20 hours. Actually I feel quite good. I am also continuing with maple syrup and baking powder. If nothing else it helps pH levels.
Further information is on the web for anyone who may be interested. I have discontinued Zoladex ADT for now. I have one 3 month injection in reserve. Meanwhile life is for living, best wishes to all.
Les
I have just taken the last dose of the first lot of 10. I have not noticed any adverse effects at all. Actually, I feel quite well. The black salve tastes terrible and looks worse. I tried it with bread but it burns my tongue for a while. Now I load a capsule using a plastic syringe just before I take it, followed by a good meal. The dose is around 0.3 cc by volume. No taste at all! At night I meditate and imagine the salve destroying cancer cells. The first pharmacy quoted 30c each for empty capsules, the second sold me 30 plus a pill bottle for $1.35. Go figure!! According to unknown internet sources I will wait 10 days before starting another course of 10. There is no science behind this. Just a hope that it will make a difference.
Best wishes to all, and thanks to all my supporters.
Les
I stopped taking the black salve 2 days ago. Last night I felt a pulsating pain in the area that was radiated for a bone metastasis earlier this year. The pain could have been due to walking, however I choose to believe it is the salve doing its job and mopping up any remaining cancer cells in that area. No one really knows how to cure cancer at this stage and I see no harm in exercising faith. I visualise the salve in my bloodstream attacking all those little buggers. I also take vitamin B1 and a multi vitamin each day. A feeling of well-being, staying positive, eating healthy foods, laughing and having supportive people around me is so important at this time.
Best wishes to all.
I have completed the second batch of 10 black salve treatments. As I have no proof of any effects, my report is purely subjective and based on my personal experience.
First 10 day period: The day after I took my second capsule I experienced some looseness in bowel movement. Otherwise, no symptoms at all for the entire period. In fact, I felt quite well.
Second 10 day period: I now load each capsule just before taking it. I increased the dosage to 0.3 cc. The day after the second capsule I was loose in the bowels again. Otherwise normal. The night after the 4th capsule I felt pain in my hip in the area where I had radiotherapy earlier this year. I was also experiencing a strong metallic taste in my mouth and I was not sleeping well. The pain continued each night for the next 3 nights and has now eased, however I can still feel discomfort. I reduced the dosage to 0.2 cc. and the metallic taste has reduced.
It has been 6 weeks since my last Zoladex was due and I am back in the land of hot flashes, most noticeable at night. No corresponding increase of libido though.
I feel positive that the salve has produced some good effects, however will not know until my next PSA in December.
Thanks and regards to fellow sufferers and to all who are wishing me well.
Life is for living!!
Les
On November 25 I took the final capsule of black salve. I had commenced 50 days earlier. My protocol was to take the capsules one per day with dinner for 10 days, none for 10 days, repeat and then the final ten for ten days. This is how it went; I felt no ill effects at any time, however I did feel some sensation around the area in my left hip where i had been radiated. I loaded 0.2cc of the salve into a gel capsule that I ate with food. I used a large plastic syringe to store and measure the salve. On the second day of each ten day group I had loose bowel motions. By the 8th day of each group I was tasting a metallic taste in my mouth that stopped when I stopped the capsules.
A few days after the final capsule I began to feel some itching in my back. I noticed there were hundreds of tiny, scabby feeling tiny sores all over my back. That would have been around December 1. The little sores spread all over my back and upper arms. They are not uncomfortable or weepy and only itch a little. They are now diminishing in number and should soon clear up altogether.
The question now is, are they due to prostate cancer cells being eliminated through my skin? I like to believe so. I had a PSA test December 16, however I cannot get the result until after January 3. I think that will tell the story.
Meanwhile, best wishes for Christmas and the new year for all of you who follow my story. Thank you for your support.
Les
Just received my latest PSA and it is 12.9, up from 3.4 three months ago. This indicates a doubling time of 6 weeks which is a bit of a worry. My doctor suggests that it may be a rebound from ceasing Zoladex, so will have another test in 2 months. I plan to contact my oncologist in Newcastle to ask his advice, and we will see what develops. As for the black salve, who knows? I remain positive at this time, still hoping it will help. Meanwhile, I am grateful for the support of all those who love me. It is too early to be making plans at this stage, so we just take life one day at a time. Otherwise I am well.
I visited my doctor last week to get the result of my testosterone test. It was zero, undetectable. It is 7 months since my last Zoladex implant so the implications are that I have been chemically castrated and no longer need Zoladex. Dr is concerned about the effects of no testosterone on bone density, muscle mass, depression, weight gain etc. I am currently 77 Kg so no concerns there. Testosterone treatments are out of the question due to PCa. On the positive, ceasing Zoladex can have had no influence on PSA, which leaves my theory that the black salve has stirred up the cancer cells. More news in March when I will have my next PSA. Meanwhile I feel fine, so staying positive.
Today received the latest PSA. 48.6. Not what I was hoping for by any means. I feel well and have no symptoms. I do tire easily, but that could be due to an ongoing sinus infection. To look at me no one would suspect that I have cancer at all. I cannot obtain treatment in Canada unless something extraordinary happens so it will soon be decision time. Do I stay and take my chances? Do I return to Australia and have treatment? I plan to have another PSA in a month and see how it trends. I have contacted my oncologist in Australia, waiting his reply. Miracles still happen, don't they?
Here I go again with the black salve, this time in capsules form. I thought it would be black but it's not, as you can see. I have read so many testimonials about black salve and other natural therapies, it is hard to accept that they are all fake. So, undaunted, I will continue in my quest for a cure, or at least a slowing down of the process.
First, to those who think I am wasting my time and money. These capsules do not cost anywhere near as much as the drugs from pharmaceutical companies. Also they do not do as much damage as chemotherapy, hormone therapy, surgery or radiation, all of which have failed in some cases despite the cost. In fact, people often end up worse off.
My new regime starts today. I take circumin with black pepper twice per day and blood root capsules 3 times per day with food, as per the manufacturers directions. I will continue to monitor my PSA on a regular basis. My last PSA in March was nearly 50 indicating a doubling time of 5 weeks. Now that is scary!
Any reasonable person would conclude that my experiment with black salve didn't work, in fact it may have made things worse! Unreasonably, I prefer to believe that it has stirred up the cancer cells, causing them to excrete PSA in their agony of dying. I visualise those little buggers writhing in pain, doubled over as PSA oozes out of their contorted bodies! The dead bodies mopped up by my strengthened immune system and leaving my body through the usual channels.
Well that is what I choose to believe. My next PSA test is later next week. Until then I hold on to my faith. Cancer does not have me. My spirit is well!
Thank you to all who consciously or unconsciously are praying for me, and a big thanks to my partner S who is my faith when mine is weak.
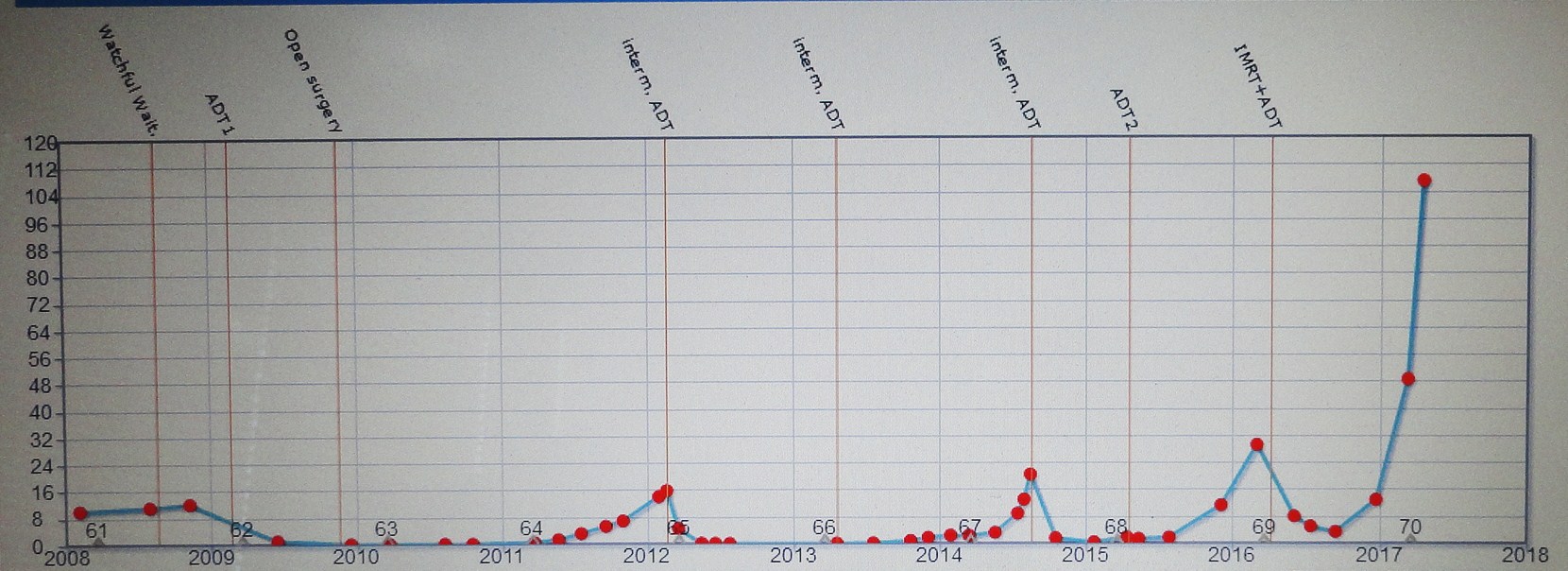
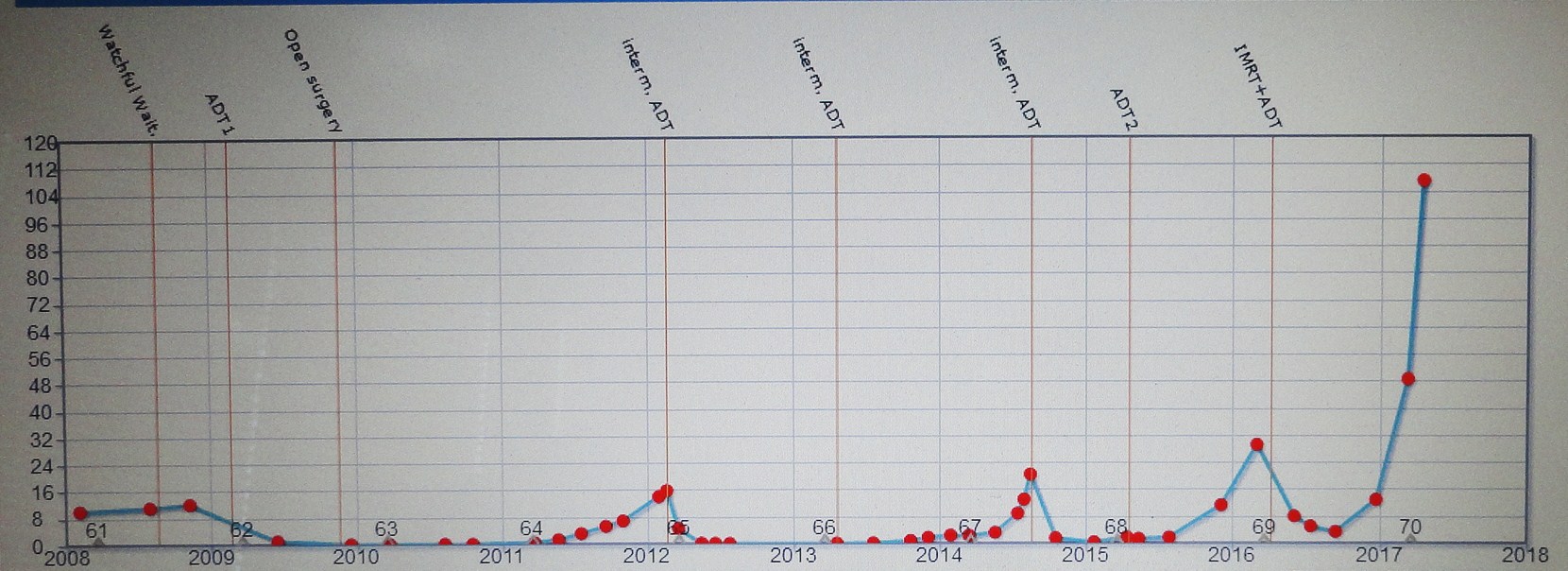
The chart says it all. PSA 107 and rising. I am returning to Australia soon and hope that my oncologist will find some kind of effective treatment. At least I can have some tests and scans to determine exactly what is going on. Talk about suspense!!
My latest PSA was 140. A week before that it was 160. Same laboratory. I have been taking Gumby Gumby in capsules. It is an Australian Aboriginal herbal remedy and it appears to be effective as nothing apart from conventional medicine has ever reduced my PSA before. I have now been referred to a medical oncologist for chemotherapy. I have yet to decide whether I will have this treatment so I have requested a second opinion re pros and cons. I don't see much point in extending quantity of life at the expense of quality, however this remains to be seen. In Australia, the government will only fund Taxotere. Other treatment options are not funded until after chemo has been tried. Even then, Abiraterone Acetate is the only approved treatment. Meanwhile I am suffering from a severe sinus infection that will only respond to surgery. I am waiting to see an ENT specialist. Thank you to all who are following my progress and praying for me. Your prayers are not wasted and I feel positive about the future.
Tuesday 15 August. The day finally arrived for the long awaited visit to the Medical Oncologist. After our previous bad experience with a registrar, we were disappointed when a young female doctor called my name. Not another registrar! How wrong we were. First she asked about my medical history and how I came to live in Canada. She discussed treatment options with insight, sensitivity and compassion.
Once she had sufficient information, including the story of how we were re-united after 51 years, she asked us to wait while she spoke to the Medical Oncologist. It turned out he is the Director of the Oncology Department and he came to see us. He explained my current status in detail and showed us the old and new psma scans side by side as he did so. He discussed treatment options and advised that as I am experiencing few symptoms at this time he feels it is too early to start chemotherapy. Apparently the Zoladex is still having a beneficial effect and he believes the sudden rise in PSA was due to me not using it when it was due.
He also said that a PSA of 140 was not a bad thing as it has been stable at that level for the past 2 months (apart from a brief spike of 160). He was very understanding about our desire to return to Canada and has supplied me with scripts for enough medication to last 6 months. Ideally he would like to see me in 3 months, but is happy for me to keep in touch via email, monitoring my PSA and advising any change in symptoms. I am to see him again in February 2018.
So, all things considered a pretty good outcome. I need to have some dental work done prior to commencing Denosumab (Xvega) injections every 4 weeks, to strengthen bones and hopefully slow down the bone metastases. I am also to continue Zoladex injections every 3 months. There is an increasing risk of hip and femur fracture so no more skate boarding for me! (Just kidding, I have never ridden one!) I am also taking Gumby Gumby daily, it is supposed to boost immunity and healing. The doctor said it can't hurt, so worth a try.
So, S and I are looking forward to returning to Canada in a few short weeks. She has been very patient and I am blessed to have her in my life. My sinuses are much improved and I am feeling much stronger. Ready for the next stage in the cancer merry-go-round.
I am very grateful for the support and prayers of so many people, people I regard as friends, all around the world. Thank you, and God bless you all.
I commenced Xgeva injections every 28 days a little over 2 weeks ago. 3 days later I felt intense pain in my left hip and by late afternoon I was convinced I had fractured something. My brother in law drove me to the Mater Hospital and x-rays showed there was no fracture. The pain settled overnight with the help of Endone (oxycodone) and Ativan (lorazepam). My GP said I should be OK to travel to Canada provided I avoid walking too much. I normally use a walking stick but still get hip and back pain. I survived the flights OK and am now back in Canada. I have been extremely tired lately and somewhat depressed, finding it hard to get to sleep without medications. I am certainly not as well as I was a year ago. The cancer has spread through my pelvis to my lower spine and also into the head of my femur. Today I bought a Rollator, or walking frame with wheels. It is very good and I can sit and rest when I need to. It takes some load off my hips and spine and distributes the weight evenly without the jerkiness of walking with a stick. I know I am on the downhill road, and I don't know how much longer I can stay active. All I can do is wait and see. I know many people are praying for my healing and I truly appreciate your prayers, but the reality is, we all have to go sometime...but, then again, it doesn't hurt to hope for a miracle!
News today is not so good. PSA is up to 392, it has more than doubled in 6 weeks. My hip and back pain levels are mostly low. I was on Norspan 5mg patches for a month but have just started oral morphine as required. Yet to see how well it works. I know people are praying for my healing, but PCa is pretty much miracle proof and we all have to go sometime. Please, if you pray for me, pray for strength and courage to face the inevitable. Meanwhile I feel well and I am active. I have lost a little weight but my appetite is good. I am in good hands and very much loved. I consider myself to be a lucky man. I am grateful to all who pray for me.
During November and December last year I was having more pain, loss of appetite and increasing fatigue. My {SA was doubling every 5 to 6 weeks, so naturally I assumed that all of my symptoms were due to spreading cancer. I would have one reasonably good day followed by 3 or 4 days bedridden. By the end of December I could not eat anything and the pain in my hip, back and abdomen was becoming unbearable. January 2, I was taken to hospital by ambulance. I could hardly stand up, I was so weak. Next day I had X-rays, blood tests and CT scans. I had my notes with me including my last psma scan on disk. The doctor said he would need to open me up to be sure about a diagnosis. Next morning I woke to find I had a colostomy bag attached to my belly. What a shock! It turns out my large bowel had perforations that had abscessed and healed over time. The infection had spread to my small bowel and abdomen. Peritonitis had set in. They removed a section of each bowel, joined the bits together and brought the end out of my belly. There were also 2 drain tubes and a large dressing. I was in hospital for 3 weeks. Toughest 3 weeks of my life. I felt like it would have been better to let me die. Stefanie was there for me every day, she bathed me, helped me pee, made my bed comfortable and comforted me. She took me home in a wheelchair as I still could not walk. Stefanie has been amazing. She has endured so much yet cared for me every inch of the way, always patient and understanding even though I was deeply depressed at times.
While I was in hospital I got connected with the cancer team, so I now have 2 oncologists, a pain management specialist and a palliative care specialist, as well as a community nursing team who came to our home to help us with ostomy management. My latest PSA was 2160. A scary number! 2 weeks ago I had a cementoplasty of my left acetabulum, or hip socket. They inject bone cement into the weak bone and it restores strength and function. I could hardly walk afterwards but now feeling much stronger and much less pain.
Some good news is that there was no cancer in any soft tissue and no impingement on my spinal cord. Radiation is still an option for my spine. My current medication is Zytiga, prednisone, Zoladex, Fentanyl and oxycodone for pain. I am slowly gaining weight. I was down to 69kg from around 80. Now up to 72kg and getting stronger each day. Next PSA a few weeks from now and hoping for a much lower number. As always, I thank everyone who is supporting me with prayers and good wishes.
Yesterday I walked 220 steps. That doesn't sound like much, does it? Even less when I tell you I used my walker. That is the longest walk I have taken this year! I was tired afterwards but it felt great to do that.
My new medication, Zytiga with Prednisone is working well so far. After 15 days PSA dropped to 1800. After 3 weeks I have no adverse side effects, just occasional hot flushes. I am also using Fentanyl patches for pain control. It is very effective with none of the side effects of morphine.
Following the cementoplasty to my left hip, my leg feels much more stable. I can walk short distances unaided but with a limp. There is no limp using the walker.
My sister Rae and brother in law Ray have come all the way from Australia and we are enjoying their company. They have rented an apartment in Richmond. We are looking forward to a 7 day Alaska cruise with them in May. Having a disability got us a really good deal, so it's not all bad!
Finally, a word on ostomy pouches. It is a smelly, messy process that still requires both of us to perform. Some days it fills up 3 times. Some days not at all. Twice we have needed to get home quickly to avoid a disaster! I expect I will soon be ok to empty the pouch on my own. I have to go down on my knees before the throne and this involves quite a bit of preparation. Changing base plates is a different story. Stefanie has that job as I can't see to make an accurate fit around the bit of bowel that sticks out of my belly. Besides I have to be on the lookout for unexpected eruptions which fortunately are rare.
The journey over the last few months has not been fun. We all hold onto life by a thread, so enjoy what you have while you still have it! Thanks everyone for your support, prayers and good wishes. They make a difference!
The latest PSA is in, 39.6! Not bad considering it was over 2000 just a few months ago. I saw my Oncologist on Wednesday to get my next supply of Zytiga and prednisone. I am so grateful it is provided for free. When I was in the hospital in January I had multiple CT scans and a bone scan. I only received the reports this month. The cancer has now spread to the neck and top region of my femur, and also into my ribs and sternum. I occasionally feel twinges of pain in my ribs. My oncologist said that I already had bad news, this is just more bad news! On the other hand there appears to be no soft tissue or lymph node involvement and no impingement on nerves in my spine, even though the tumour in L4 has grown larger. I still feel well and able to walk, although I worry about how much longer my femur will hold out. We are entering the end game, I know that and I have to be realistic about it. I am not so worried for myself, I worry about how it affects the people I love, and the ones that care about me. For now the Zytiga is working and PSA is falling. The cancer is slowing down and that means I get to live a bit longer!
Thursday 2 August latest PSA reading is 14.7. 4 weeks ago it was 19.7 and up until now it has consistently halved each month, so this reading, around 75% is a little disappointing. The good news though is that it is less than last time so I will take that gratefully.
Meanwhile I am continuing with the Zytiga and Prednisone with no apparent side effects apart from growing pert little breasts. My testosterone is virtually undetectable at less than 0.1. The good thing about that is that it starves the tumours and slows down any growth. The bad is that it takes away all sexual urges, then again maybe that is not so bad as nothing works down there anyway! My rib still aches at times and I take Tylenol in addition to the Fentanyl patches every 3 days. I notice the rib pain more on the third day.
The ostomy is still troublesome at times. It is always there except for a few hours every 4-6 days when I remove it to replace it. I like to just relax and give the skin some air for a while. I know it is not polite conversation to talk about one's bowel habits, but when it is right in front of you it is hard to ignore. Most times when the bag is removed I can collect any "output" in a tissue and then put it in a plastic bag. Last time, this was working quite well until suddenly there was a lot of gas, causing S to leave the room and then an increase in "output" causing me to hastily fit a new skin barrier and pouch. Luckily I got it on in time and didn't make a mess, however the new bag quickly filled up. Should have waited, but that is ostomy care. Full of surprises!
However, life is good and I am glad to be alive. I have been following the Golden Globe Race and have found a program that will allow me to virtually enter the race. Haven't tried it yet so that is a subject for another blog at a later date.
It's the end of yet another month. This month of August 2018 is special in a couple of ways. Firstly it marks 10 years of survival from my initial diagnosis when my PSA was 12. Secondly my latest PSA has finally dipped below 10, coming in at 9.2, so I am pretty pleased with that. Full credit for the improvement in my PSA must go to what I call The Awesome Four. Four little (not so little) Zytiga tablets ($50 each if I had to pay for them!) that I take every morning followed by prednisone.
I feel good. I am fit and strong, walking well (with the aid of my trusty walker). The worst side effect is that my skin is becoming very thin and I bruise and bleed easily. However, that is a small price to pay for the resulting PSA drop. What does lower PSA actually mean though? It means that the cancer tumours will be less active and less likely to spread. Unfortunately it does not mean there will be less cancer, so I still need to be careful to avoid falls or heavy loads on my legs.

The cross stitch is progressing well. I am quite pleased with it and only a few thousand stitches to go and then the detailing and rigging to finish. I need to consider how I am going to frame the finished work and I have a few ideas. S has a love for the Waratah, an Australian native flower of striking beauty (just like her!) and that will be the subject of my next project.
Meanwhile life goes on. Mr Dumpy (colostomy bag) has been up to his usual tricks. I really need to get my diet under control. Multigrain bread and carbonated drinks cause havoc. Today, while out shopping, I suddenly realised that Mr Dumpy had filled almost to bursting point with gas. I was driving and so could not relieve the pressure, an operation that requires me to get out of the car. (It stinks!) I told S, "One more fart and it's all over!" However, it held out until we got home.
Sadly, my Mum passed away a few weeks ago. She was 95 and had lived a full and enjoyable life. She said she was ready to go and after a short illness she left this world in her sleep. Unfortunately I was not able to travel to Australia to see her or attend her funeral. A generous relative held her phone up for the entire service, allowing us to watch live. The wonders of modern technology!!
So this month has been a mixture of good and not so good. Life goes on and so do we.
There is no easy way to say it...after 8 months on Zytiga my PSA has stopped falling at 9.2 and has now risen to 10.2 in 5 weeks. Does this mean Zytiga has failed? I don't know to be honest and I must admit it scares me to think what might come next. I have been feeling pain in my ribs and discomfort in my sternum lately despite the Fentanyl. I take Tylenol occasionally when needed, otherwise I still feel well. I am still gaining weight, now 87 kgs. A little more than ideal. I walked nearly a kilometre today with my trusty rollator. I saw Dr Ho this morning and he said that it is possible the PSA will continue to fluctuate around the current level and it does not necessarily mean that the treatment has failed. I hope he is right. If the next PSA rises significantly I will probably have another bone scan. Chemotherapy doesn't appeal to me, however I have read that some people have had good results without too many bad side effects, so never say never. Each month when I go for a checkup I see the people receiving chemotherapy sitting in their armchairs and I wonder what it must be like for them. I am reminded that I am not the only victim of cancer and that really I have had it pretty good compared to some people. I have survived 10 years from diagnosis and I have lived more than 70 years. I don't have to worry about losing my marbles in later life. My next PSA is in 3 weeks. Can't wait to see the score!
Got the news last Wednesday...PSA is up to 16.7 from 9.2 a month ago. I saw my oncologist today and he said he is disappointed. Me too, I said. It seems likely that the Zytiga is no longer working. We will persist for another month and if still rising I will have some scans and possibly back to the radiation oncologist. I am still recovering from kidney stones and it has not been the best couple of weeks. I also had my 3 monthly Zoladex injection. The nurse said she hates doing Zoladex injections. It is a huge needle that injects a pellet into my abdomen. What about me, I said!
I am still trying to figure out how I feel about it all. Chemo was mentioned and dismissed. Dr Yun also mentioned a radiation treatment involving infusion of radioactive material into the blood stream (lutetium?) I did some research and it seems BC Cancer Agency is planning a trial next year and I may qualify. Preliminary tests have shown great promise. A radioactive isotope targets cancer cells and destroys them while leaving healthy cells alone. There is still some hope. Google "Lutetium PSMA" for more information.
Next week I will have another bone scan. At least it will give us a picture of where the bone metastases are.
There are things I would still like to see and do. I need to prioritize because there is no way I can do them all. Most important at this time is to finish 3 tapestries, maybe 4 or 5 if time permits. Physical activity tires me quickly but needlework calms and distracts me.
I need to downsize as well. I plan to edit my many hours of video into something watchable. I want to post some of my life on YouTube, maybe someone will enjoy it. A video review of my life for my funeral is another project. I am fortunate that I have time to prepare. I am not afraid to die. What concerns me is that I will miss out on seeing some exciting things, such as great grandkids. Sometimes I feel as though it is up to me to make people feel ok when the subject of cancer comes up. I am still me and I will be til the end. Having cancer sorts out the real friends and I am blessed that I have Stefanie, family and friends who will stand by me. I thank God for such people.
Up at 6.0am this morning for the slow wet drive into Vancouver in the dark. I don't think the sun came up at all today and it's still raining.
We saw Dr T. and what a change! Whenever we have seen him before he was abrupt, clinical and in a hurry to finish. Today he was totally opposite. The results. The bone scan shows more activity as expected. PSA is up to 20.2, not bad considering.
He discussed 2 options, chemo and radium 223. Radium 223 (Xofigo) is 6 injections of a radioactive isotope that finds rapidly dividing bone cells and kills them. It is not a cure but can give an average additional 3 to 4 months of quality life compared to doing nothing. The injections are 4 weeks apart, cost $5000 each and are flown in from Europe. I would be radioactive, especially Dumpy would be, but not a danger to others and I quote "providing it is not swallowed"!!
The other treatment, chemo, he said would have similar effectiveness re survival time, however, he minimised the side effects. He said the cancer is confined to bone, though if it metastasizes to soft tissue (liver or lymph nodes) radium 223 can't be used. I asked him what would he do if it was him? He said he would have the radium 223 and then he could have chemo later if need be, but not the other way round. Sounds reasonable to me.
He also discussed giving a single shot of radiation to treat a spot on one rib that gets painful at times. Next it was off to x-ray. They took about 15 x-rays of my ribs, hips and legs. I will see Dr Y. next week and hopefully he will show us the scans and x rays.
Meanwhile I am still feeling reasonably well apart from some blood pressure issues, very high, due to Zytiga. I get tired very quickly and I don't seem to have the energy I had in the summer. I will have to stop Zytiga before starting the radium223, so hopefully the blood pressure will improve. So, another decision to be made re treatment choices. I suspect I will go with the Radium223.
On the last day of 2018 we saw Dr Tyldesley. PSA is up to 46 which means it is back to doubling every five weeks. He showed us the recent bone scan and an x ray. The cancer has spread to some more ribs and also my spine. The main concern however is that now my right femur and right side of the pelvis have significant cancer and there is an increased risk of fracturing my legs. He even mentioned the possibility of inserting rods as a preventative measure, however he thinks the radium therapy might be enough at this stage.
On the second day of 2019 it was back to the Vancouver General Hospital for the radium injection. First we saw a second radiation oncologist who is also a nuclear medicine specialist. He trained in Philadelphia, lectures at the University of British Columbia and also spent 2 years in Brisbane. He explained the process in detail and answered all of our questions. We both feel very confident with this man even though we don't recall his name. He did mention that the treatment could be continued beyond 6 months if it is beneficial.
Next was the injection. First they inserted a canular into my arm and connected it to a saline drip. Then comes the radium solution in a syringe which is carried inside a lead container. The solution is then injected slowly into the IV line. I felt no immediate effects. So now I am radioactive. The half life is 10 days. The radioactivity is highest for the first week and any excess is excreted through feces and other body fluids.
Next week it is back to the cancer clinic for a CT scan and more radiation.
After that, who knows? Today I have had a couple of dizzy spells. Is it the radium? Is it due to changes in medications, or none of the above? Time will tell. For now it is fingers crossed and hope for the best.
My second Radium 223 infusion was just 3 days ago and right now I am feeling rather crappy, tired and nauseated. Is the cure worse than the disease? It isn't even a cure, just buys a bit more time. I have to wonder if it is worth the trouble. I had 5 medical appointments last week, I feel like a voodoo doll. At the beginning Dr T, radiation oncologist said that R223 would probably not reduce PSA but should prevent it from rising too much. The good news is that the PSA has dropped dramatically from 46 to 35. Funnily enough I felt better when my PSA was over 2000! Dr T also said it is normal to feel pain after the infusion. He was right about that. After the first infusion I slipped getting out of the bath. Next day the pain in my back was almost unbearable despite the Fentanyl patch. It took 4 oxycodone a day for 4 days to control the pain and then it just stopped. I am to have an MRI sometime soon. Just as I was starting to feel better it was time for the second infusion. Two days later the pain came in my sternum and ribs. Fortunately it only lasted one day. So, I plan to continue to endure this treatment for the time being in the hope that things will improve.
It has been quite a trying week for both of us. First was the news that my PSA has risen from 35 to 63.4, not what we were hoping for. We saw Dr T on Tuesday at BCCA. I was very tired following the MRI on Monday. I had to lie on the examination bed so I wouldn't faint. Dr T said that the MRI looked ok but he doesn't have the complete report yet. We discussed the rising PSA and he said it looks like perhaps the radium is not working, however he would like me to continue with the radium treatment. We discussed my fatigue, apparently radium does not usually cause such fatigue. Next it was up to the lab for more blood tests and an ecg (electro cardio gram). It was good to get home. The radium infusion was to have been on Wednesay but Dr T has rescheduled it for Friday. Dr T called next morning and said my electrolytes were out of whack and I am dehydrated, which would contribute to me feeling dizzy and faint. I had the option to go in for an infusion or dehydrate according to his recommendations. I was already taking electrolytes every second day. He suggested l take Hydrolyte daily and double my water intake. After drinking more water and increasing the electrolytes I did feel better on Wednesday and we managed to go out for lunch. I even had a short walk around the shops so it was a good day. Today we saw Dr Y who was his usual cheery self. I said I was concerned about the rising PSA. He said that "sometimes when cancer cells are dying they give off a lot of PSA, text book." Then he said, "don't give up yet, I will tell you when to give up....never!" Tomorrow is the third radium infusion....We wait and see how it goes. Must say I have been better since increasing fluids and electrolytes though. Meanwhile the remaining snow is slowly melting away.
Dr T was on leave last week so we saw a Dr D instead. This month my blood markers were all within the normal range indicating no problems with liver and kidney function or bone marrow. However there is some concern about my PSA, now up to 107 from 96 4 weeks ago. The concern is that the Radium is no longer effective, however I believe it is slowing down the rate of PSA increase. Some specialists think that increasing PSA is an indicator to cease radium treatment. After the 3rd infusion PSA increased by around 50%. After the 4th infusion the increase was around 12%. So that must mean something. I was given the option to discontinue radium therapy if I wished. I asked him about Lutetium trials but he said i would not qualify. He suggested that we speak to Dr Y about possible clinical trials and any other available treatments. After we came home I phoned Dr Y. He advised that as the radium was "holding back" the cancer to some extent it would be wise to continue the full course. It appears that the only other options available to me after that would be some form of chemotherapy. Before that can happen I need to be rid of all traces of radium. I have mixed feelings about chemotherapy. Would I be sacrificing quality of life for a few extra months? How well would I tolerate side effects? I have heard good and bad stories about chemotherapy. It sounds like a bit of a lucky dip, but then such is life. Maybe I will give it a go. I can always pull out if I want to. At least I will have given it a try. I have to say, I really don't know what PSA numbers really mean. It seems they bear no relationship to how I feel or what I can or can't do. The fact that the rate of increase in PSA is reducing makes me think that the Radium treatment is just now having a positive effect. I have read where patients have given up after 4 treatments. Maybe they gave up too soon. Anyway this is something we will discuss with the nuclear medical oncologist. On the subject of how I feel, I have good days and bad days. That is too simplistic. "Good" days are days when I don't feel nauseous or light headed, I can walk to the car and enjoy an outing of 3 to 4 hours, and I feel like eating. They are fairly rare and very unpredictable. "Fair" days are probably most common. On fair days I wake up feeling ok but not fancying breakfast so I have a protein drink. If I walk to the car (about 100 metres) I usually feel dizzy by the time I get there. I feel slightly nauseous with little appetite. I can enjoy doing cross stitch as I can do it while resting in bed. "Crap" days are fairly common too. On crap days I can do a bit of cross stitch or watch tv. I feel nauseous and dizzy when I get up. I often need an afternoon nap even though i might have slept 12 hours, and my appetite is very poor. "Really crap" days are fortunately rare. On these days I feel impending doom, I can only pick at food and I begin to wish it could all be over. I lose interest in everything. It is really hard to describe and I don't wish to sound morbid but it is what it is. Fortunately these days are rare, but when they coincide with medical appointments it is all I can do to get there and back. Without S to help me I wouldn't be able to go. She drives, she helps me with my walker. She holds my hand and encourages me to keep going. She makes sure I am nourished. It is impossible to predict what tomorrow will be like. All we can do is enjoy the good days, make the most of the fair days and endure the crap days. Don't worry, life is still worth living and there is always hope that tomorrow will be a good day!
We saw Dr Yun today and I had yet another Zoladex injection. Yesterday was my last radium infusion. PSA was up to 179 from 107 4 weeks ago, so that is a concern. Basically it means the radium is not working any more. The recent CT scan shows no soft tissue metastases and that is a great relief. There are however, signs of skeletal advancement but that was expected. So far no signs of fractures and I am being very careful not to slip or fall as a hip fracture would be disastrous. All the doctors agree that chemotherapy would be the next option. They are looking at commencing treatment (Docetaxel) in about 5 to 6 weeks. I still feel life is worth living so I have decided to give it a go and see what happens. I can always quit if I want to. I plan to write to Dr Wratten and ask his advice as returning to Australia is still an option. Meanwhile I have increased my prednisone and I have noticed some improvement in how I feel. Better to be fat than miserable. Next week I will be back on Zytiga for 4 weeks and it will be interesting to see if any effect on PSA. It is just a waiting game, meanwhile we enjoy the good days and endure the bad ones. I still enjoy and benefit from my needlework, and of course there is always Netflix!
My latest PSA is 242. Two weeks ago it was 247, so it has decreased a little with no special treatment. I started chemo (taxotere) today. I said in the past that I would never have chemotherapy as I preferred quality of life to quantity of life. I have been researching taxotere and it seems improvements in managing side effects and better control of administration of the drug has led to better outcomes. In fact some of the stories are very positive. I am being closely monitored and I can withdraw from treatment any time I feel it is not for me. The only effect I have noticed so far is a slight dryness in my mouth. I wish to thank all who support and pray for me. I do appreciate it.
Chemo number 2 has been delivered and this time I feel so weak and lethargic, out of sorts. It is hard to get interested in anything for long and when I get up I feel wobbly and shaky. A couple of nights ago I got up to go to the bathroom and felt very faint. As I staggered back to bed I passed out, banging a rib on furniture as I fell. I have a sore rib as well as the chemo effects. And I took some skin off. My mouth is still very dry and I have bad breath due to the damage to my mucous membranes. However this will soon pass and I expect to feel better in a few days. Latest PSA is 290, up by 48 from last time. This could be due to dying cancer cells giving off PSA. Anyway I will hang onto that for now. I fancied Chinese today so Stefanie brought home some takeaway which I really enjoyed. So the plan for now is to continue the treatments and hope for a good result.
The 4th chemotherapy session did not go well. The nurse had a lot of trouble finding a vein and the infusion took much longer than usual. The after effects were no easier to put up with and when the PSA came in it was still 500. Chemotherapy is not working and so, I will not continue with it. Quality of life is more important than quantity. 2 weeks later, the side effects are mostly gone. We met with Dr Y and I advised him that I did not wish to continue with the chemo. I also advised him that we are returning to Australia and my oncologist Dr W, at the Mater Hospital. Dr Y was supportive and optimistic as usual. He agreed that future treatment options are limited and he offered to provide a full medical history with a CD of any medical imaging for Dr W.
My sister and her husband spent a few days visiting and asked if they could meet Dr Y. He was very gracious and answered my sister's questions. They have generously offered to let us stay with them in their home, for which we are deeply grateful. We fly out in 6 weeks with a rest stop in Honolulu as I don't think I could endure doing the trip in one go.
Besides, I have never been to Hawaii!!
Leslie's e-mail address is: roosterpig47 AT gmail.com (replace "AT" with "@")
NOTE: Leslie has not updated his story for more than 15 months, so you may not receive any response from him.