 Adenocarcinoma:
is used to describe epithelial tissue in a gland that has become malignant. It
is identified in a pathology laboratory and given the name of the tissue affected.
e.g. the prostate gland tumor gets the name 'prostate adenocarcinoma', because
its cells resemble the cells of the prostate.
Adenocarcinoma:
is used to describe epithelial tissue in a gland that has become malignant. It
is identified in a pathology laboratory and given the name of the tissue affected.
e.g. the prostate gland tumor gets the name 'prostate adenocarcinoma', because
its cells resemble the cells of the prostate.
 Prostate Cancer. Frequently referred to as PCa, PC or CaP. As those who have
been following the steps recommended in this part of the site - going from DON'T
PANIC through SOME GOOD
NEWS! to here - will be aware, there are many varieties of prostate
cancer. Most are a slow growing cancer and there is usually an ample amount of
time to research available options. No one diagnosed with PCa should have to undertake
treatment until they understand what the treatment involves and what the outcomes
and side effects of the treatment will be. One of the RECOGNIZED
EXPERT PATHOLOGISTS is Dr. Jonathan Oppenheimer who has this to
say:
Prostate Cancer. Frequently referred to as PCa, PC or CaP. As those who have
been following the steps recommended in this part of the site - going from DON'T
PANIC through SOME GOOD
NEWS! to here - will be aware, there are many varieties of prostate
cancer. Most are a slow growing cancer and there is usually an ample amount of
time to research available options. No one diagnosed with PCa should have to undertake
treatment until they understand what the treatment involves and what the outcomes
and side effects of the treatment will be. One of the RECOGNIZED
EXPERT PATHOLOGISTS is Dr. Jonathan Oppenheimer who has this to
say:
For
the vast majority of men with a recent diagnosis of prostate cancer the most important
question is not what treatment is needed, but whether any treatment at all is
required. Active surveillance is the logical choice for most men (and the families
that love them) to make.
GLEASON
GRADES AND SCORES
If
prostate cancer cells are discovered in the biopsy material, they are evaluated
using a scale known as the Gleason Grade (GG) which was established in the 1960s
and which had five grades. As explained above, the pathologist or technician would
look for the patterns in first (prime) focus making up more than 50% of the sample
of the cancerous material. Patterns that were well differentiated, but abnormal,
were graded as 1; at the other end of the scale, poorly differentiated patterns
were graded as 5. Healthy glandular tissue is well differentiated, so a Gleason
Grade of 5 is "bad" news: a Grade of 1 is "good" news. A similar
approach is applied to the second (secondary) focus with abnormal glandular patterns
making up less than 50% of the sample. No attention was paid to a third (tertiary)
focus initially
After
each focus was graded, the primary and secondary Gleason Grades are added
together to establish a Gleason Score (GS). The Gleason Score therefore
was a scale that ran from 2 (1+1=2= "good") to 10 (5+5=10=("bad").
Typical examples of Gleason Scores would be shown as GS 3+2=5 or GS 3+3=6. These
were the most common scores until the end of the last century. A Score of 6 was
the midpoint in the overall scale. It is important to note the difference between
a Gleason Grade and a Gleason Score (which is the sum of the Grades.)
Since
the advent of PSA testing in 1987 there has been a gradual change in the interpretation
of Gleason Grades starting in 2005. The changes were formally recognized
in January 2010.
 Grades 1 and
2 are no longer labeled as adenocarcinoma or cancer in material obtained through
a needle biopsy.
Grades 1 and
2 are no longer labeled as adenocarcinoma or cancer in material obtained through
a needle biopsy.
 It is recommended
that some material that was previously graded as Grade 2 should now be graded
as Grade 3 and some material previously graded as Grade 3 should now be graded
as Grade 4. This means that from the time the changes were made a Gleason Score
of 6 (3+3) is the entry level for a positive diagnosis. Previously it was the
midpoint on the overall scale.
It is recommended
that some material that was previously graded as Grade 2 should now be graded
as Grade 3 and some material previously graded as Grade 3 should now be graded
as Grade 4. This means that from the time the changes were made a Gleason Score
of 6 (3+3) is the entry level for a positive diagnosis. Previously it was the
midpoint on the overall scale.
 Some tunors with
a Gleason Score of 5(3+2) previously will now have a Gleason Score of 6 (3+3):
some which had a Gleason Score of 6 previously will now have a Gleason Score of
7.
Some tunors with
a Gleason Score of 5(3+2) previously will now have a Gleason Score of 6 (3+3):
some which had a Gleason Score of 6 previously will now have a Gleason Score of
7.
 Since some of
the new Gleason Score 7 tumors will have an outcome more similar to Gleason Score
6 tumors, a some distinction is made between a Gleason Score of 7a (3+4) and 7b
(4+3).
Since some of
the new Gleason Score 7 tumors will have an outcome more similar to Gleason Score
6 tumors, a some distinction is made between a Gleason Score of 7a (3+4) and 7b
(4+3).
These
changes make some comparisons between current studies and old studies more difficult.
The
Gleason Score is a critical item that drives much of the decision making process.
Grading biopsy samples is a subjective process. Numerous studies show that agreement
on Gleason Scores will only occur in about 35% of cases, with roughly equal Scores
higher and lower than the original Score. It is very important to get a second
opinion on the material from any biopsy procedure from a RECOGNIZED
EXPERT before making any final decision on treatment.
For
more detailed information go to GLEASON
GRADES. BOB
PARSONS wrote an excellent piece analysing his biopsy slides and
including some good images of them. Although I labeled it BOB
PARSONS' PATHOLOGY 101 it may be a little advanced for a newly
diagnosed man.
STAGING
The
final part of an initial diagnosis is to stage the disease. This describes the
estimated extent of the cancer or the degree to which it has progressed. The old
system had four stages - ABCD to describe the progress of the disease but the
currently recommended system is known as the TNM system. The details can be read
at this link STAGING SYSTEM.
The main features are:
 T refers
to the estimate of the amount of tumor within the prostate. There are four main
T stages each with three subsets. The most common staging is T1c which means there
is a tumor present, found in a needle biopsy performed due to an elevated serum
PSA but not detectable clinically or with imaging. A T2 staging is the next most
common and would refer to a tumor associated with a positive DRE. T2 tumors are
thought to be contained within the prostate gland.
T refers
to the estimate of the amount of tumor within the prostate. There are four main
T stages each with three subsets. The most common staging is T1c which means there
is a tumor present, found in a needle biopsy performed due to an elevated serum
PSA but not detectable clinically or with imaging. A T2 staging is the next most
common and would refer to a tumor associated with a positive DRE. T2 tumors are
thought to be contained within the prostate gland.
 N refers
to the status of the lymph nodes near to the prostate - whether the prostate cancer
has spread there or not. It is unusual to see any N status other than NX - cannot
evaluate the regional lymph nodes.
N refers
to the status of the lymph nodes near to the prostate - whether the prostate cancer
has spread there or not. It is unusual to see any N status other than NX - cannot
evaluate the regional lymph nodes.
 M indicates
if the disease has metastasized. As the tumor grows within the prostate it may
start to spread beyond the prostate gland and capsule to more distant parts of
the body. The cancer sites away from the prostate are called metastasized sites
- sometimes referred to as secondaries or more commonly 'mets'. The most common
M stage is MX - cannot evaluate distant metastasis.
M indicates
if the disease has metastasized. As the tumor grows within the prostate it may
start to spread beyond the prostate gland and capsule to more distant parts of
the body. The cancer sites away from the prostate are called metastasized sites
- sometimes referred to as secondaries or more commonly 'mets'. The most common
M stage is MX - cannot evaluate distant metastasis.
The
result of the staging is a formula such as cT2aN0MX. This would indicate a tumor
in half or less than half of one of the prostate gland's two lobes with no sign
of spread to the lymph nodes and an inability to ascertain the presence or absence
of any metastasis.
The
initial staging is known as the clinical stage and is signified by the letter
c in front of the formula mentioned above - the most common staging being cT1cNXMX
or cT1cN0M0. This means that on initial examination the tumor is not detectable
clinically or with imaging and there is no evidence of spread beyond the gland.
If
the gland is removed in surgery, another pathology report is prepared. The pathological
staging is usually different to the clinical staging and is prefixed by the letter
p. There may be significant changes in the staging which is one of the main reasons
for having surgery. A clearer picture is obtained. The pathological staging for
example might go to pT2cN1M0 - the tumor is in both lobes; there has been spread
to the regional lymph nodes; there is no distant metastasis.
It
is important to understand the difference between clinical and pathological staging
if any of the various tools - such as the Partin Tables mentioned below - are
used to try to estimate outcomes. The data in those tables is usually based on
clinical staging. After an initial diagnosis is made, a number of further tests
and scans may be ordered. The data from the diagnosis may also be used in the
various calculators or nomograms that have been developed to try and predict the
outcome of the diagnosis or treatment options.
SCANS,
TESTS AND CALCULATORS
After
an initial diagnosis is made, a number of further tests and scans may be ordered.
The data from the diagnosis may also be used in the various calculators or nomograms
that have been developed to try and predict the outcome of the diagnosis or treatment
options.
SCANS
Scans
are done in order to try to establish what, if any, spread there is into or beyond
the prostate capsule. The benefit of some of these scans is doubtful in many cases.
Some leading practitioners consider the automatic ordering of CAT and bone scans,
which occurs frequently, as a waste of money. Their necessity should be established
before the scans are undertaken.
The
Partin Tables (described further on) can help in making this decision. The chances
of there being metastases to the bone are remote with a small volume, low-grade
(Gleason Grade 6) tumor However, there is a high correlation between high Gleason
Grades (8 and above), a large tumor and the extent the disease has moved beyond
the gland. According to one leading authority there is virtually no possibility
of metastasis occurring until the tumor reaches a critical volume of about 12
cc. The average prostate gland has a volume of about 25 gm, so in this view about
half the gland would be occupied by cancer cells before metastasis occurred. In
such a case there would usually be a positive DRE (Digital Rectal Examination)
and a palpable mass. A leading expert has also expressed the view that metastasis
will not occur if the PSA is less than 50 ng/ml, unless the Gleason Score is very
high - greater than 8.
X-RAY
It
was standard practice to order X-rays as a matter of course on diagnosis. However,
the chances of any signs of spread being shown, using X-rays alone, are slim.
Since it is more usual to run other scans, there is little point in having an
X-ray. Many people strongly believe in avoiding any unnecessary exposure to X-ray
to minimize the chance of cell damage.
CT/CAT
SCANS: MRI SCANS
Although these two scans CT/CAT (Computer Axial Tomography) and MRI (Magnetic
Resonance Imaging) use differing technology, they are similar in the the sort
of output they produce. Both create a series of images, in effect showing views
of the organ being examined in "slices". The CAT scan uses X-rays to create the
images. The MRI scan uses a very strong magnetic field for this purpose. The MRI
images can be enhanced by the use of an endorectal coil. This is a small device
inserted into the rectum, which generates secondary fields.
Both
examinations can be a little intimidating for those having them for the first
time. The person being scanned lies on a small trolley, which enables them to
be moved into a large cylindrical structure containing the scanning machinery.
There is very little room in the older cylinders, especially for larger men, and
a feeling of claustrophobia can result. Newer machinery has more room. The MRI
process is noisy and operators should provide earplugs or headphones. Most men
do not have signficant pain from either procedure - just a degree of discomfort
from remaining immobilized during the scan, and the noise - but this is not always
the case.
Some
experts feel that CAT scans are only of value in the diagnostic process of advanced
prostate cancer, which is usually associated with PSA readings of 50 ng/ml or
higher and Gleason Scores greater than 8. CAT scans are highly insensitive in
detecting disease in the lymph nodes, and valueless in most patients in detecting
penetration of the capsule, which is usually the first stage of progression of
the disease. MRI scans with the endorectal coil can be much more useful but even
then will only be associated with an accuracy rate of between 75% and 90%. Both
types of scan have high false positive and false negative results. In other words
they will identify tumors which don't exist or miss ones which do exist.
There
are several other scans in use. Two for which claims are made of greater accuracy
are the COLOR-DOPPLER
and the Ferraheme. The former is not available in many institutions. It combines
two forms of scan - Ultra Sound and MRI to produce an image that, it is claimed,
show a more precise picture of any areas likely to contain cancer cells. The two
best known practitioners being Duke Bahn at Community Memorial Hospital, Ventura,
California and Fred Lee at Crittenton Hospital Medical Center, Rochester, Michigan
who can be seen talking in THIS
VIDEO. Ferraheme has yet to be approved by the FDA and is based
on the COMBIDEX
scan. The manufacturers of Combidex could not get FDA approval in the United States
and production of the scan has ceased. The Ferraheme scan is used, still in an
experimental mode, at SAND
LAKE IMAGING in Florida.
BONE
SCANS:
Bone
scans fall under the general term of nuclear medicine. The way in which these
scans work is the reverse of a CAT scan or an X-ray. In those examinations, the
radiation is sent out of a machine through the patient's body. Nuclear medicine
examinations, however, use the opposite approach. A radioactive material is introduced
into the patient's body (usually by injection), and is then detected by a machine
called a gamma camera in the case of the bone scan.
The
procedure for a bone scan involves nuclear material injected into a vein (usually
in the arm). There is a wait of two to three hours for the material to circulate
in the system. The person being examined then lies on a special table and the
gamma cameras (one above and one below) slowly track down the length of the body.
The entire procedure takes between 30 and 60 minutes. Bone metastases are usually
associated with advanced prostate cancer, so bone scans are not considered essential
for early stage disease. For men with a PSA of less than 10 and a Gleason Grade
of 6 or less, the chances of the disease having metastasized to the bone has been
estimated at less than 1% - which is equivalent to zero in medical terms.
Some
people are concerned about the introduction of nuclear material into the body,
but it is said that the radiation from this procedure is similar to that from
a normal X-ray. The material is quickly cleared from the body. There is nothing
painful about the procedure - apart from the injection, but having to remain motionless
for the time of the scan can be a little uncomfortable.
PET
SCANS
A
PET (Positron Emission Tomography) scan is also a nuclear medicine imaging test
in which a small amount of liquid radioactive material is injected into your body.
It is claimed that they can identify soft tissue metastases more accurately than
other scans. PET scanners are now commonly combined with computed tomography (CT)
scanners, called PET-CT scanners.
As
is the case with the bone scan you will have to wait for about 90 minutes after
the liquid radioactive material is injected. It may be necessary to drink some
contrast material that moves through the stomach and bowel and helps to improve
the interpretation of the scan. Occasionally, depending on the medical indication
a catheter may be placed into your bladder to help improve image quality. Positioned
on the PET scanning bed, it is important to remain as still as possible during
the scan as movement can result in reduced image quality and the images may be
blurry.
If
you are having a PET-CT, the CT scan is performed first and takes less than 2
minutes. The PET scan takes approximately 30 minutes but the time will vary depending
on the regions of your body being scanned.
OTHER
TESTS
There
are two other tests that have been used in the past but which are often ignored
now and one new test. Whilst none of these tests is definitive, all can give a
little added information to help in the process of assessing status before determining
strategy. The older tests are the DNA ploidy and PAP (Prostatic Acid Phosphatase)
tests; the newer one is the PCA3 test.
PCA3
ASSAY
The
PROGENSA PCA3 assay is a urine based test that identifies the level of a genetic
component that is often present in prostate cancer. It was approved by the FDA
(Food and Drug Administration) in the United States in February 2012 and has been
in use in Europe for some time. The primary use of the assay is to assist in the
identification of cases where a biopsy procedure is justified because of an elevated
PSA or where an elevated PSA has resulted in a negative biopsy. Because the PCA3
assay result is said to be unaffected by BPH (Benign Prostate Hyperplasia) cells,
it is claimed that when used in conjunction with PSA tests, it may give a better
indication as to whether prostate cancer is present despite negative biopsy results.
The assay should not be used for men with atypical small acinar proliferation
(ASAP) on their most recent biopsy.
One
of the drawbacks to the use of the assay is that there is a requirement that the
prostate gland be "massaged vigorously" in order to get a viable result.
There may be physical problems in achieving this and it may be difficult to have
a consistent understanding of the term 'vigorous'.The clinical study of the PCA3
assay upon which FDA approval was given only included men who were recommended
for repeat biopsy. Therefore, the performance of the assay has not been established
in men for whom a repeat biopsy was not already recommended.
DNA
PLOIDY
DNA
ploidy is another test that may indicate the potential aggressiveness of a tumor
and its likely responsiveness to androgen deprivation therapies. Ploidy is a term
used to describe the chromosome content of the cell population of a tumor. Diploid
cells have normal chromosome pairs and normal DNA. They tend to grow slowly and
respond well to hormone therapy. Aneuploid cells have abnormal numbers of sets
of chromosomes. They tend to be more aggressive and not to respond as well to
hormone therapy. Aneuploid tumors are more often associated with high Gleason
score prostate cancer (8-10) and non-organ confined prostate cancer. The ploidy
test may not be done by all laboratories, but is done by Bostwick, one of the
laboratories recognized as being a RECOGNIZED
EXPERT PATHOLOGIST.
PAP
(PROSTATIC ACID PHOSPHATASE)
The
PAP (Prostatic Acid Phosphatase) test is a blood test that may be an indicator
of early metastasis (spread of the cancer) although only 75% of patients with
metastases have an elevated PAP. Few doctors seem to be aware of the potential
value of the test and may dismiss PAP as having been replaced by PSA as a prostate
cancer indicator. Like many other tests, it may be worth tracking PAP results
over time. Persistently elevated levels - 3.0 or higher - are cause for further
investigation and may indicate that surgery is not the best option.
CALCULATORS
There
are tables and nomograms that are used to try to calculate the likelihood of the
spread of PC out of the capsule of the prostate using your PSA, Gleason Ratings
and Staging. Although they look complicated at first, they are understandable
with a bit of patience. As part of your to gain a better understanding of your
condition you should do your best to do this. The PARTIN
TABLES prepared by the Brady Urological Institute was one of the
first calculators and gives a very good explanation. It allows you to make your
own calculation of the probabilities. To do this you will need your clinical staging,
your PSA and your Gleason Score. Other calculators are listed on the PALPABLE
PROSTATE site. Some of these are more complex than the Partin Tables
and need more information concerning your diagnosis.
GLOSSARY
We
have only listed some of the most common terms. There are many comprehensive
Glossaries on the Internet giving many more of the terms used. Here are two good
ones:
SUMMARY
The
process of diagnosis can be a frightening and stressful experience for most. Tests
are ordered, often without any apparent reason or explanation; results are given
in language that is difficult to interpret or understand; and all the time the
fear grows. Hopefully, this section will take some of that fear away. There is
also often a feeling that time is limited, that a decision regarding treatment
must be made very soon after diagnosis. For the vast majority of men the window
of opportunity for successful treatment is a wide one and decision-making may
safely take many months.
THREE
IMPORTANT FACTS ABOUT TESTS
There
are three basic but important facts about all medical tests:
ACCURACY
 The first important
fact - No test is 100% accurate. Diagnosis is not an exact science.
The first important
fact - No test is 100% accurate. Diagnosis is not an exact science.
The
degree of error can vary considerably, depending on the complexity of the test
- and some tests are very complex indeed. Sophisticated machinery is used for
some - the maintenance of the machinery can alter the result. Chemicals are used
in other tests - the use-by date or source of these chemical agents can alter
results. Technicians run the tests - their training can alter results. The outcome
of all tests needs to be interpreted by a specialist - their expertise can vary.
All this adds up to a degree of uncertainty and explains why it is very important
to have all results checked by the most knowledgeable person available - and why
second opinions should be sought automatically.
CHANGES
 The second important
fact - The value of many of the medical tests lies in measuring the change in
the results, not in the results themselves.
The second important
fact - The value of many of the medical tests lies in measuring the change in
the results, not in the results themselves.
The
most obvious example is the PSA test. It is important to measure the size and
speed of any change, since this gives an indication of the aggressiveness of the
disease. To get this measurement it is necessary to have a series of tests at
regular intervals. This may mean delaying the start of treatment but the information
is invaluable. This same concept applies to other tests.
MISTAKES
 The third important
fact - mistakes can be made.
The third important
fact - mistakes can be made.
The
medical world does not differ from any other place. Human beings run it and they
can make mistakes. Get copies of all test results - ensure they are yours. If
an unusual result does not relate to other results, have a re-test in case a mistake
has been made, before taking immediate action.
When
you go to the next step you will see what we believe are actions you need to take
to enhance your chances of survival.
NOW
GO TO STEP 4 - SURVIVING PROSTATE
CANCER



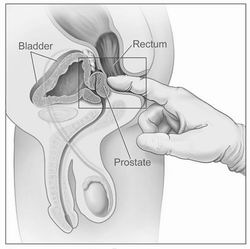 Because
the prostate gland is so well hidden, the only way it can be physically examined
by your doctor is via the rectum. If you have an understanding of where the prostate
is located, it is pretty obvious that this is the only way it can be reached.
The doctor inserts a finger to feel the prostate - trying to establish whether
there is anything unusual about the gland: a firmness or softness perhaps, or
nodules, or roughness on the surface. A biopsy may well be ordered if the DRE
reveals any abnormal features even if there is no elevated PSA.
Because
the prostate gland is so well hidden, the only way it can be physically examined
by your doctor is via the rectum. If you have an understanding of where the prostate
is located, it is pretty obvious that this is the only way it can be reached.
The doctor inserts a finger to feel the prostate - trying to establish whether
there is anything unusual about the gland: a firmness or softness perhaps, or
nodules, or roughness on the surface. A biopsy may well be ordered if the DRE
reveals any abnormal features even if there is no elevated PSA.